Young patients with spinal tumors could be good candidates for radiosurgery, study suggests
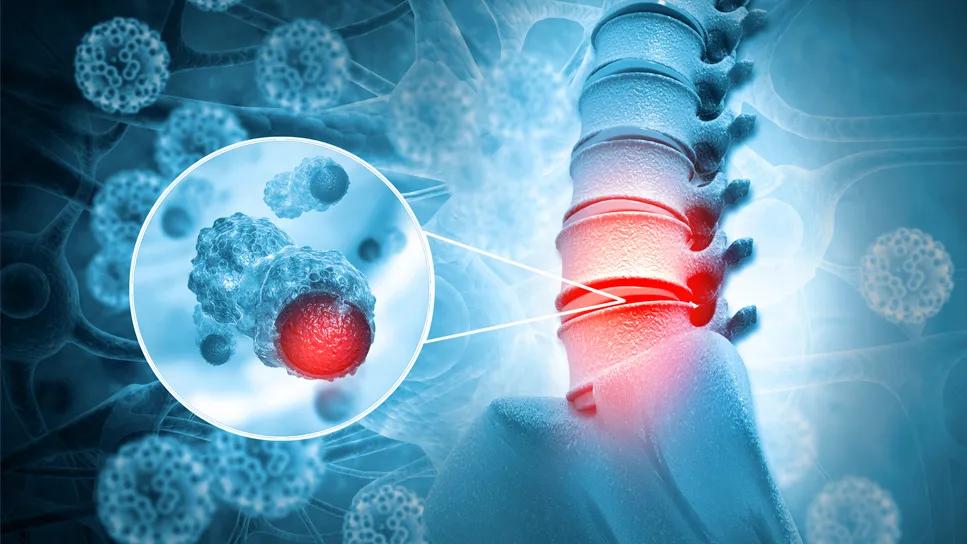
Spine stereotactic radiosurgery (SRS), which delivers a high dose of precisely targeted radiation to attack hard-to-treat spinal tumors, has become a common therapy for adults. However, even though adolescents and young adults have shown a high tolerance for aggressive treatment in the past, it has not yet become the standard of care for younger patients with metastatic sarcomas in the spine. Now early results from a study provide some of the first data showing that such patients are able to tolerate SRS for these types of cancers.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The findings offer hope to a patient population that often comes to radiotherapy after multiple rounds of chemotherapy and prior radiation, making them at high risk for side effects, says Erin Murphy, MD, Director of Pediatric Radiation Oncology at Cleveland Clinic.
SRS offers major advantages for adolescent and young adult patients. It utilizes higher doses with multiple beams tightly aimed at the target site, reducing damage to surrounding tissue and minimizing radiation exposure. And since it can be delivered in just one to five sessions (fractions), it is far less disruptive to the patient’s school schedule and activities than conventional radiation therapy, which may require daily sessions for several weeks.
Treatment is more complex and requires greater planning. Patients must be immobilized in a specific position that can be reproduced for each session. During the session, treatment is guided by real-time imaging and patients must be immobilized in a specific position so that the position can be reproduced for each session.
The new study, published in JNS Spine, looks at seven patients with metastatic Ewing sarcoma or osteosarcoma with a total of 11 spine lesions treated with SRS at Cleveland Clinic. Patients ranged in age from 15 to 26 years, with a median age of 20.3 years. Irradiated sites included the thoracic, lumbar and sacral spine, and the median dose delivered was 35 Gy in five fractions.
Within the study follow-up period, eight of the 11 treated lesions remained locally controlled for a median duration of 11.1 months. Treatment was well tolerated overall. While one patient developed grade 3 gastrointestinal toxicity, the patient’s treatment overlapped with a round of intense chemotherapy, which is a known risk factor for increased toxicity.
Advertisement
“The key takeaway is that patients actually tolerated these treatments really well, but you had to be very thoughtful about the concurrent therapies that are given,” Dr. Murphy says.
A secondary finding was that patients with larger tumors, paraspinal masses or epidural disease benefitted more from a fractionated course of treatment.
“These are small numbers and an early experience,” Dr. Murphy acknowledges, “but we thought it important to get it out there and share what we’ve learned from looking after these patients.”
Researchers are now conducting prospective trials to gather data on outcomes for adolescents and young adults being treated with radiosurgery for metastatic sarcomas. One question Dr. Murphy hopes to study is how SRS interacts with the patient’s own immune system to fight tumor cells. She also called for more clinical trials to better understand the right radiation dose and how radiosurgery can best be used in conjunction with other therapies.
“We can take a lot from our adult experience in doing spine radiosurgery, but we certainly know that these are different patient populations with different tumors and different chemotherapies and probably different immune responses,” she says. “So it’s both an exciting time but also a very challenging time, because there’s still a lot to learn.”
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors