Elevated levels of vWF and FVIII associated with risk of blood clots, severe COVID-19 and death
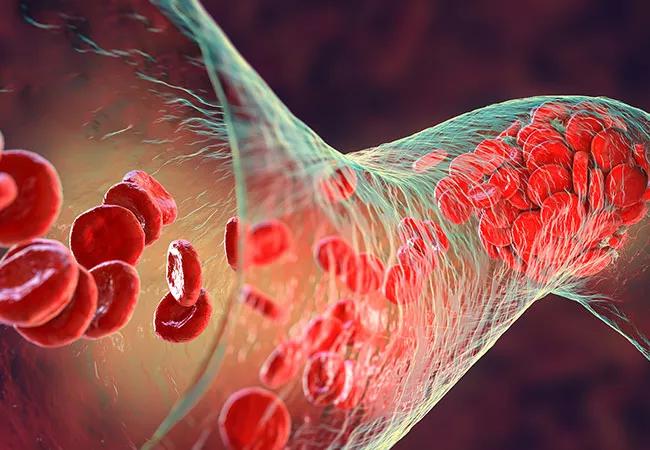
Patients with cancer are at elevated risk of blood clots. Does that mean COVID-19, which has also been associated with blood clots, raises that risk even further? The answer, according to a new study, appears to be no. However, the same study identifies surprising biomarkers that could be used to identify which patients are at the highest risk of COVID complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We don’t currently have a good biomarker for bad outcomes for cancer patients with COVID,” says Alok Khorana, MD, a physician in Cleveland Clinic’s department of Hematology & Oncology, and lead author on the study. “This could be a way to differentiate them for closer monitoring or interventions, using labs that are already available in every hospital.”
The study, “Hemostatic Biomarkers Predict Risk of Thromboembolism (TE): Severe COVID-19 and Mortality,” was presented at the 2022 American Society of Hematology (ASH) annual meeting.
The research grew out of the ongoing National Cancer Institute COVID-19 in Cancer Patients Study (NCCAPS), Khorana said. As researchers were looking at thromboembolism outcomes, Khorana reflected that these events only represented “the tip of the iceberg.”
“If thrombotic events are more likely in patients with cancer, that must mean the coagulation system is even more activated than it usually is,” he says. “That’s what led to not just looking at the clinical events, but also at the subclinical symptoms, including the activation of coagulation and platelets, and whether that was associated with better outcomes.” For the study, researchers followed 1,619 patients with cancer who were diagnosed with acute COVID-19. A sub-cohort underwent testing for a range of hemostatic biomarkers.
Scientists found that, overall, patients with cancer and COVID-19 had a 3% risk of developing thromboembolism within 30 days of being diagnosed with COVID-19. “Patients with cancer are already at high risk for blood clots, so this doesn’t raise it much more beyond that,” says Khorana. However, they also found that elevated levels of two biomarkers that signal activation of the hemostatic system: Von Willebrand Factor (vWF) and Factor VIII (FVIII) were associated with increased risk of thromboembolism. They were also strongly associated with risk of severe COVID-19, as well as increased 90-day mortality from any cause.
Advertisement
“I was surprised at the strong association of these two factors with the three complications, because the complications are not really linked,” Khorana says. “It suggests that there are underlying inflammatory hemostatic pathways that are contributing to each of these conditions.”
As for why the overall risk of thromboembolism was not higher, Khorana explained that the apparent lack of elevated risk likely reflects risk levels that changed over the course of the pandemic. While initially patients with cancer did see higher levels of thromboembolism, those numbers went down with different COVID-19 variants and with the advent of vaccines.
Next, Dr. Khorana plans to look at long-term biomarker changes in patients with cancer diagnosed with COVID-19. Researchers also plan to do a deeper analysis on their data and look at how it changed over the course of the pandemic to determine whether different strains of COVID-19 affected results.
Advertisement
Advertisement

Dynamic modeling improves the accuracy of outcome predictions for ICU patients

A review of IDSA and NIH guidelines

Study sheds light on how clinicians addressed their patients’ pain and insomnia during the pandemic

Patients report improved sense of smell and taste

Clinicians who are accustomed to uncertainty can do well by patients

Unique skin changes can occur after infection or vaccine

Will enable patients with long COVID to enroll in national clinical trials

Cleveland Clinic analysis suggests that obtaining care for the virus might reveal a previously undiagnosed condition