Highlighting treatment gaps and challenges in the management of rare condition
Findings from an administrative health claims-based dataset provide valuable insight into idiopathic multicentric Castleman disease (iMCD) in the U.S. This analysis, presented during the 2024 American Society of Hematology conference, showed that siltuximab—the only FDA-approved treatment for this condition—was used in just 22% of patients. This reveals a significant unmet treatment need, considering this is the only FDA-approved drug for iMCD in the U.S.
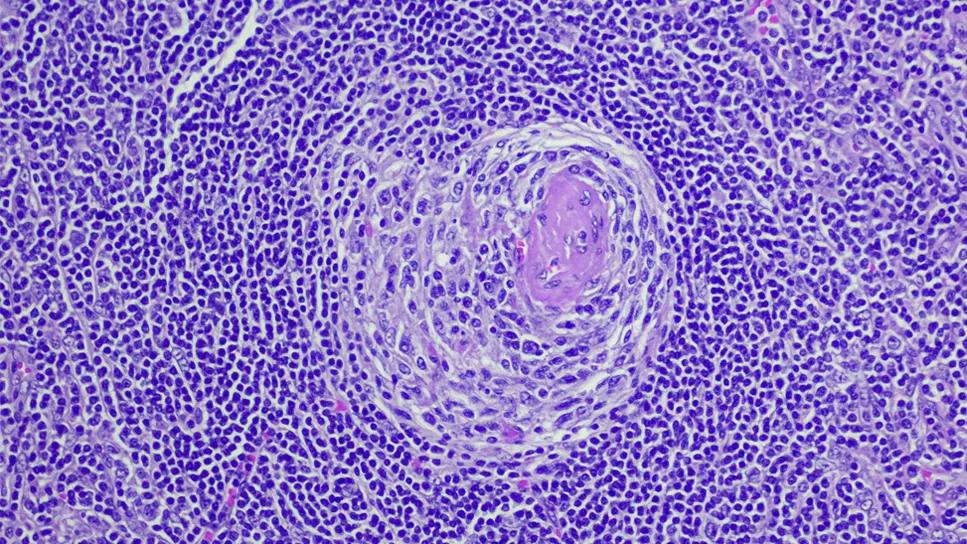
“Idiopathic multicentric Castleman disease, or iMCD, is an exceptionally uncommon condition,” notes study author Sudipto Mukherjee, MD, PhD, MPH, with the Department of Hematology and Medical Oncology at Cleveland Clinic Cancer Institute. “The epidemiology of iMCD remains incompletely understood due to its rarity, complex diagnostic criteria and poor reporting due to the absence of an ICD diagnosis code until 2017. More recently, findings from U.S. administrative health claims datasets and disease registries in the U.S., China, Japan and Europe have been helpful in estimating the incidence and prevalence of this disease. However, there still remain knowledge gaps in the U.S. This hinders accurate assessment of disease prevalence, natural history and treatment patterns.
“Knowing the magnitude of the disease burden is essential, especially now that we have an FDA-approved treatment that has proven remarkably effective for iMCD patients,” he continues. “Understanding the prevalence and natural history of the disease has significant implications for early and accurate diagnosis and the timely initiation of treatment. This was the driving force behind our study.”
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Unlike more common cancers, such as breast, colon or lung, which are reported to registries using International Classification of Disease (ICD) codes, Castleman disease did not have an ICD-10 code until 2017.
“This made it nearly impossible to estimate how many people were diagnosed with or living with the condition in the U.S.,” explains Dr. Mukherjee. “The introduction of the ICD-10 code has transformed our ability to study iMCD, providing an unprecedented opportunity to understand its epidemiology.”
For this study, Dr. Mukherjee and colleagues used an administrative health claims dataset particularly because health claims data offer a detailed view of the disease’s clinical and natural history, including office visits, hospitalizations, diagnostic tests, procedures and treatments. These details allowed the research team to analyze how patients are managed, the treatments they receive, how long they stay on therapy, disease- and/or treatment-related outcomes and whether they experience delays in treatment.
“One of the major challenges of studying iMCD is that the disease has many mimics, falling into three broad categories: autoimmune conditions, other cancers and infections,” says Dr. Mukherjee. “To classify a patient as having iMCD, it is critical to rule out certain infections (e.g., HIV, HHV-8), malignancies and autoimmune diseases.”
In their analysis, the investigators looked at health claims-based data from 2016 to 2023, comprising 66 million patients. To identify iMCD patients with the highest level of diagnostic certainty, the investigators developed a novel algorithm that incorporated ICD-10 diagnostic claims for CD, international evidence-based diagnostic criteria and treatment claims for the recommended or most commonly used therapies for iMCD.
The methodology behind this research is quite novel. After identifying the pool of CD patients and excluding those with HIV/HHV-8 infections, the investigators used three key strategies to identify iMCD patients as well as capture the prevalence, treatment patterns and gaps in care of these patients:
• Identifying CD patients who met the minor diagnostic criteria for iMCD
• Identifying CD patients who received treatments such as siltuximab that are recommended for iMCD
• Combining these two criteria, classifying patients as iMCD if they additionally met the minor diagnostic criteria for iMCD or had accompanying claims for routinely used iMCD-specific therapies.
Patients with conditions mimicking Castleman disease, such as autoimmune diseases (lupus, rheumatoid arthritis, Sjogren’s) and certain cancers (mainly lymphomas and myelomas), were excluded to enhance specificity.
Advertisement
The investigators analyzed data from the MarketScan® by MerativeTM Commercial and Medicare administrative claims database, covering the period from October 2016 to July 2023. Among 816 HIV-/HHV-8- patients with a Castleman disease diagnosis, 251 (31%) were identified as potential iMCD cases.
Of these patients,155 of 251 (62%) were defined by minor criteria only, 41 of 251 (16%) were identified by treatment only, and 55 of 251 (22%) met both minor and treatment criteria. After excluding patients with CD mimics consistent with diagnostic criteria, the investigative team identified 186 iMCD patients. The mean age of iMCD patients was 49 years, and 52% were male.
Only 22% of identified iMCD patients had claims for siltuximab, despite its status as the only FDA-approved treatment for the disease. Additionally, 16% of patients received rituximab, a non-FDA-approved alternative recommended by the National Comprehensive Cancer Network (NCCN).
“Our analysis underscores the exceedingly rare nature of iMCD. Even more striking, only about 20% of these patients received siltuximab,” notes Dr. Mukherjee. “Ideally, all 186 patients should have been treated with this drug, but the vast majority were not, highlighting a significant unmet treatment need.”
This is particularly concerning because untreated iMCD can lead to severe complications, including high rates of organ dysfunction (kidney and lungs), blood clots and secondary cancers. Without timely treatment, iMCD patients can become critically ill or even die.
“Addressing this treatment gap is crucial. The medical community needs to prioritize raising awareness among physicians and the general public, promoting early diagnosis and ensuring patients receive FDA-approved treatments in a timely manner,” says Dr. Mukherjee. “There is no reason for patients to miss out on a proven therapy when it is available.”
Advertisement
Another key takeaway from the research is the broader applicability of the study methodology. Using novel algorithms, the researchers effectively leveraged health claims data to study the epidemiology of iMCD, offering a template for investigating other rare diseases. “Our approach provides a feasible and adaptable framework for researchers studying similarly rare conditions, helping to advance understanding and improve patient outcomes across various fields,” Dr. Mukherjee suggests.
Building on this research, Dr. Mukherjee and his colleagues plan to explore the economic burden of managing and treating iMCD. “Siltuximab is administered once every three weeks for the rest of a patient’s life,” he says. “The cost can quickly become overwhelming, especially for those without insurance. Patients, insurers and physicians need to be aware of the financial burden associated with treatment.”
The investigators also plan to take a closer look at the impact timely treatment has on the development of complications. “If we can demonstrate that timely treatment reduces the likelihood of these complications, it would send a powerful message that early, FDA-approved therapy is essential for modifying the disease’s natural history and preventing long-term health issues,” Dr. Mukherjee concludes.
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient