Emerging field enables treatment tailored to each patient
Lymphedema was considered an untreatable condition until relatively recently. Modern advances in reconstructive microsurgery and supermicrosurgery have turned lymphedema into a condition that can be surgically managed; however, very few surgeons are trained to perform these advanced procedures.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
When associated with breast cancer treatment, lymphedema is a chronic and progressive swelling in the upper extremity ipsilateral to the axillary node dissection or site of radiation treatment. Patients may present with swelling in the upper extremities, skin changes, stiffness and paresthesia. The timing of disease progression varies from patient to patient and is dependent on a variety of factors, including the severity of the initial lymphatic injury. Historically, lymphedema was considered to be only treatable with lymphedema therapy; there were no surgical options. However, promising advancements in super microsurgery make it an option for select patients.
Traditionally microsurgery represents the most delicate surgery possible. The lower limit of microsurgery is 0.8 mm, so anything smaller than that was out of reach prior to supermicrosurgery.
Supermicrosurgery was developed at the University of Tokyo in 2000 by Professor Isao Koshima, MD, as a technique for anastomosing vessels smaller than 0.8 mm. For many years, Professor Koshima was the only surgeon in the world to perform the technique. Supermicrosurgery spread to the United States about a decade later, although the term itself was formally adopted at the First European Conference on Supermicrosurgery in Barcelona in 2014.
“Supermicrosurgery is a rapidly evolving field. In 2014, the lower limit for vessels was 0.3 mm. Today, we’re down to 0.1 mm. The number of surgeons who can perform supermicrosurgery is growing too. There are now a dozen across the country, with three at Cleveland Clinic, including Risal Djohan, MD, Graham Schwarz, MD, and myself,” says Wei Chen, MD, FACS, Head of Regional Microsurgery and Supermicrosurgery, Co-Director of the Center for Lymphedema Research and Reconstruction in the Cleveland Clinic Department of Plastic and Reconstructive Surgery.
Advertisement
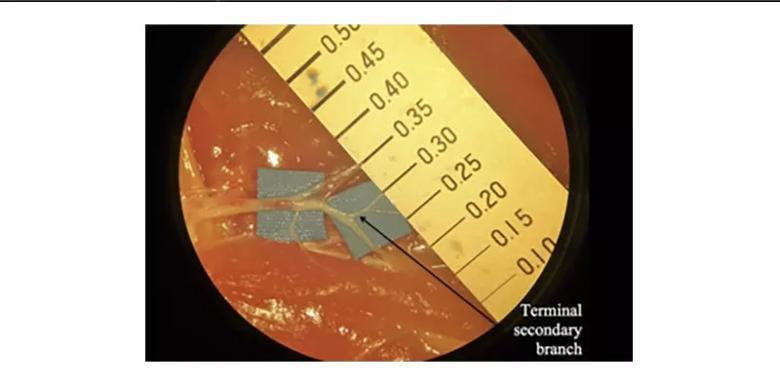
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/36faf64a-5bd5-4104-affc-66377230a678/20-PSX-1047-supermicroLymphTerminlSecondBranch-inset-800x397-1_jpg)
These vessels, found in chicken thighs, are appropriate for training for supermicrosurgical lymphaticovenular anastomosis. Image repurposed with permission; originally published here: Chen WF, Eid A, Yamamoto T, Keith J, Nimmons GL, Lawrence WT. A novel supermicrosurgery training model: The chicken thigh. JPRAS Open. 2014:67;973-978.
“In addition to treating lymphedema, supermicrosurgery is also used in other reconstruction (e.g., a non-healing wound in a patient with advanced diabetes). In the past, these patients would have required amputation. Now, with supermicrosurgery, we can save these legs,” Dr. Chen continues.
In the United States, the commonly preferred procedure is lymph node transfer. “At Cleveland Clinic, however, we believe that all procedures are valid and that treatment should be individualized,” Dr. Chen says. Cleveland Clinic offers the full spectrum of procedures for the treatment of lymphedema, preventive lymphaticovenular anastomosis (LVA), therapeutic LVA, lymph node transfer, lymph vessel transfer, lymphedema liposuction and radical excision.
“From my experience, I think there really isn’t one single procedure that allows optimal treatment for every patient. Different procedures have different risk and benefit profiles, so we tailor treatment and surgical recommendations depending on an individual patient’s condition,” says Dr. Chen.
The supermicrosurgery team at Cleveland Clinic is known as a leader in the field, and receives requests for advice and instruction from around the world, according to Dr. Chen. “We typically do a virtual visit for this type of consult. So far, we’ve had a 100% conversion rate from the initial virtual visit to a physical consult.”
Advertisement
“All surgeries carry the risk of complications — we weigh the risks and benefits of a procedure for each patient. In the case of lymph node transfer, we cause lymph injury in one part of the body to treat it in another. This drawback alone negates the benefits of the procedure in my mind, and that is what motivated me to seek a better option,” Dr. Chen states.
In search of a better option, Dr. Chen and colleagues created a new technique called vascularized lymph vessel transfer (VLVT), which may be appropriate for patients with fluid-predominant disease and advanced lymphatic injury. Currently, Dr. Chen is the only surgeon in the United States performing this procedure; however, it is already being picked up in Europe and Japan.
In VLVT, following lymphographic mapping of the lymph vessels and Doppler perforator mapping, a thin superficial iliac artery perforator flap is harvested to recruit the lymph vessels while preserving the lymph nodes.
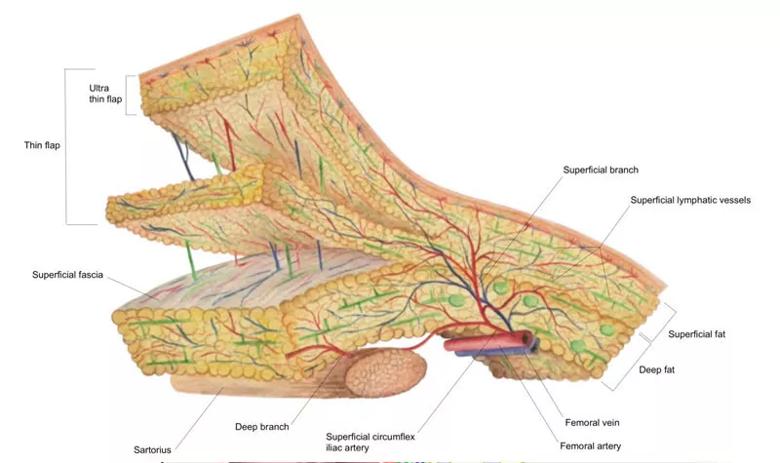
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/10562594-ccd4-4e2a-83a8-4ee2984c108b/20-PSX-1047-supermicrosrgyLymphedema-inset-800x475-1_jpg)
The SCIP-based VLVT flap was typically harvested immediately superficial to the Scarpa’s fascia to preserve the lymph nodes that are anatomically situated deep to the Scarpa’s fascia. This creates a thin flap that facilitates flap inset. In obese patients, the above technique would produce a thick flap. In these patients, we harvested the flap along a non-anatomic, artificially created plane created at 3-5 mm under the dermis. SCIP, superficial iliac artery perforator; VLVT, vascularized lymph vessel transfer. Image repurposed with permission; originally published here: Chen WF, McNurlen M, Johnson D, Bowen M. Vascularized Lymph Vessel Transfer for Extremity Lymphedema – Is Transfer of Lymph Node Still Necessary? Microsurgery. 2019;3(3):1.
Advertisement
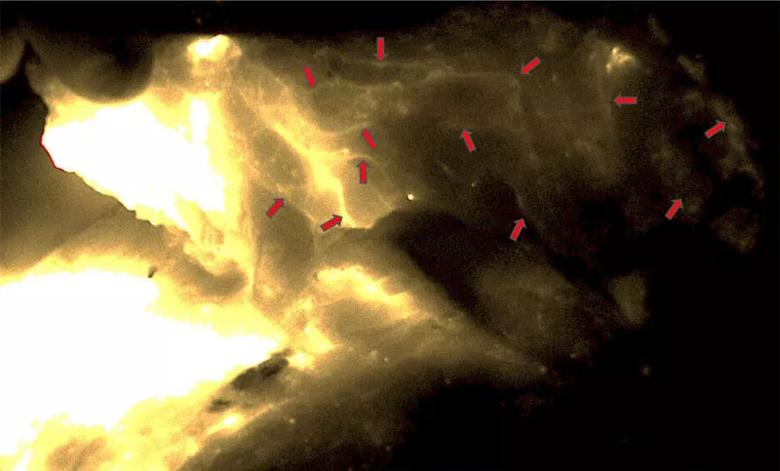
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3fac39aa-3e47-4ca2-bd24-050e7766a345/20-PSX-1047-supermicroLymphNetwork-inset-800x483-1_jpg)
Dense lymphatic network seen in the VLVT flap (red arrows). The image was taken from the adiposal side of the flap. The bright areas on the left side represented the ICG injection site. No lymph nodes were seen in the flap. ICG, indocyanine green. Image repurposed with permission; originally published here: Chen WF, McNurlen M, Johnson D, Bowen M. Vascularized Lymph Vessel Transfer for Extremity Lymphedema – Is Transfer of Lymph Node Still Necessary? Microsurgery. 2019;3(3):1.
For patients with lymphedema of the arm, the SCIP flap is transferred to the wrist using the radial artery as the recipient vessel. Preferentially, the flap is vascularized with perforator-to-perforator anastomosis.
LVA is a delicate supermicrosurgery technique performed under powerful magnification to ensure safe suture of miniscule vessels. To ensure that LVA is achievable for patients with advanced disease, Dr. Chen developed a technique that he calls “Octopus LVA.” Octopus LVA achieves LVA in situations in which the standard technique would not be successful. In octopus LVA, incisions are placed over healthy lympograhpic patterns, and dissection is performed through 2- to 4-cm incisions under x18 to x20 magnification. Lymphatic vessels with sufficient quality between the superficial and deep fasciae are skeletonized and anastomosis is performed to create a LVA complex or octopus. Compared to traditional LVA, the octopus technique is less technically complex, less expensive and takes less time.
According to Dr. Chen, supermicrosurgery demands rigorous coordination between the eye, microscope and hand, as well as dexterous handling of delicate tissues. Dr. Chen believes that, given the right training, a resident can pick up the necessary skills to perform supermicrosurgery in three months, and is currently testing this hypothesis. “If we can [successfully train new surgeons], it would be a very meaningful contribution to our field. Those of us already practicing microsurgery and supermicrosurgery are very passionate about these techniques. But they can be intimidating to a more traditionally trained plastic surgeon. I hope that if we alleviate some of the fear and hesitation by showing that trainees can become full-fledged supermicrosurgeons in a relatively short period of time.”
Advertisement
Advertisement

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units