Two-stage procedure capitalizes on liver's ability to regenerate

An innovative surgical treatment option that leverages the liver’s regenerative capacity is showing promise for some patients with previously unresectable liver metastases from colorectal cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The two-stage surgery, known as Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS), makes it possible to treat patients who are not appropriate candidates for traditional liver resection due to multicentric disease and an inadequately small future liver remnant.
When both lobes contain tumors, hepatobiliary surgeons and radiologists in Cleveland Clinic’s Liver Cancer Program work together to identify the lobe with the lower tumor burden. After excising the lesions in this lesser-affected lobe, the true novelty of their approach begins. They simultaneously enhance the growth of this lobe while working to shrink the contralateral lobe — the one with the greater tumor burden – so that it can be more easily resected during a follow-up procedure.
“The ALPPS procedure allows us to treat patients who have a substantial amount of tumor, with both lobes affected by tumor,” says Federico Aucejo, MD, Director of the Liver Cancer Program, Surgical Director of the Liver Tumor Clinic and Co-Director of the Liver Tumor Center of Excellence.
In the first stage of ALPPS surgery, at the same time that surgeons resect the metastases from one lobe, they ligate the portal vein supplying blood to the other. They also partition the liver with a transecting incision of the parenchyma to interrupt intrahepatic vascular connections. This approach serves a dual purpose – starving the metastatic hemi-liver of its blood supply while diverting as much as possible to the lobe that will be preserved.
Advertisement
Partitioning the liver helps enhance growth of the future liver remnant by stimulating increased expression of growth factors and cytokines and inducing hyperplasia, Dr. Aucejo explains. “This not only makes the lobe of the liver grow larger, but does it faster.”
“We can then perform the second and larger operation, where we remove the contralateral side — the lobe with the greater tumor burden,” he says. The second stage typically is performed one to two weeks after the first operation.
Preoperative computed tomography shows extensive bilobar liver metastases from colorectal cancer.
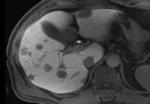
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/efcbdd08-e027-4b2a-ad1c-526ba5de707f/Fig2-150x104_jpg)
First-stage hepatectomy to clear metastases from the left lateral segment.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4b02a7aa-50db-4628-85c4-96a33f7167e6/Fig3-Labled-150x104_png)
First-stage hepactectomy showing left lateral segment after metastases resection.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7bff39b5-b4f9-493a-b4b1-8e519fbc8d5a/Fig4-Labeled-150x102_png)
First-stage hepatectomy showing ligation of right anterior and right posterior portal veins.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/32fa0efd-64d0-41aa-8620-a3986870d4dc/Fig5-Labeled-150x104_png)
First-stage hepatectomy showing transection of the liver.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c495f7f8-7ee0-4908-9b18-9cf77507da52/New-image-of-liver-transection-150x104_jpg)
Second-stage (extended right) hepatectomy. (Extended right hepatectomy). The future liver remnant is the left lateral segment cleared of metastases.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ec3e619e-7c75-4999-8df2-063f06ef40ec/Fig8-150x104_jpg)
Resected extended right lobe.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f8ac678c-6c47-4f87-8fc4-5e990a904a19/Fig9-150x104_jpg)
CT scan after second-stage hepatectomy, showing enlarged left lateral segment without radiologic evidence of tumor.
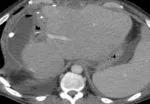
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f3dff3a3-ec82-435b-86d8-e0d7868570f5/Fig10-150x104_jpg)
Portal vein embolization (PVE) is another method to convert unresectable bilobar cancer into resectable by inducing hypertrophy of liver segments. Following excision of the small metastatic lesions in the future liver remnant, rather than surgical ligation of the portal vein, interventional radiologists perform peri-operative embolization (using a percutaneous catheter to deliver embolic agents to occlude the vein), redirecting portal blood to the future liver remnant.
Advertisement
A distinct advantage of occlusion is less manipulation of the local anatomy. “When we come back for the second stage of the procedure, we find virgin tissue there,” Dr. Aucejo says. “Generally, there is less inflammation, and dissection of the tissue is easier.”
Interventional radiologists also can perform a venous deprivation technique. In addition to cutting off the blood flow to half the liver, they embolize the hepatic vein coming out of the same lobe. “That allows for substantial atrophy of that lobe and substantial growth of the contralateral lobe, the one that we are going to leave in the patient,” Dr. Aucejo says.
Physicians in the Liver Tumor Cancer Program have performed about 10 ALPPS and venous embolization/deprivation procedures to date. Whichever approach is used, preserving at least 30% of total liver volume is the mandatory safety margin. In terms of patient selection, patients 60 years old or younger generally have better outcomes with these two-stage interventions.
“This surgical technique is applied in very select patients,” Dr. Aucejo says. “But it clearly opens an opportunity for improved patient survival when there are no other alternative treatments.”
For example, recently an out-of-state colorectal cancer patient with extensive bilobar metastases that were not amenable to traditional resection sought a consult with Cleveland Clinic. “After evaluating the liver volumetry and tumor burden affecting both lobes, I decided to offer an ALPPS procedure, as it was the best possible option to clear the liver from disease,” Dr. Aucejo says.
Advertisement
Months after surgery, the patient developed a small recurrence in the remaining liver that was treated with external beam radiation. “As of today, the patient is back to his home town, reconnecting with his normal life and family”, Dr. Aucejo says.
Cleveland Clinic is one of the few centers offering a comprehensive range of advanced techniques to treat complex liver cancer cases.
They require “a high level of surgical expertise,” Dr. Aucejo says. “ALPPS is a valuable part of a comprehensive toolkit we have to treat these patients, which includes systemic treatment, surgical therapies and interventional radiology strategies. Despite the evolution of non-surgical treatments when surgical options are not possible, five-year survival ranges between 10 and 20%, as opposed to 30 to 60% when surgery can be performed.”
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors