Autoimmune disease may have effects beyond brain, retina & inner ear
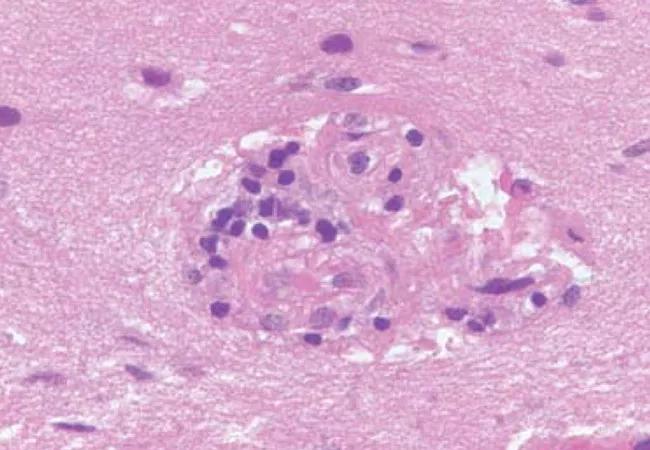
Susac syndrome (SuS) is a rare autoimmune disease that affects the microvasculature of the brain, retina and inner ear. The immunopathogenesis is thought to be similar to that of juvenile dermatomyositis (JDM), an autoimmune occlusive microvascular endotheliopathy that causes microinfarctions in the muscle, skin and gastrointestinal tract.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Clinical symptoms of SuS include uni or bilateral visual field defects, hypoacusia, headache, confusion, memory impairment, changes in behavior, ataxia, bladder dysfunction, vertigo and dysarthria. “Snowball” lesions are typically found in the corpus collosum on brain magnetic resonance imaging (MRI).
According to Robert Rennebohm, MD, of Cleveland Clinic’s Susac Syndrome Consultation Service, SuS primarily affects people between the ages of 18 and 40 (although 11 percent of cases have been reported in children and adolescents), with a ratio of 2 females to 1 male. “A little over 300 cases have been reported in the medical literature, but the prevalence of SuS is believed to be much higher largely due to the propensity for misdiagnosis,” he says.
Although the natural history of the disease is that it eventually resolves and remits, it can cause irreversible damage. Hence, early diagnosis and treatment are essential to improved outcomes and quality of life. Few clinicians are familiar with the disease, but the symptoms overlap with other syndromes commonly seen in rheumatology practice. As such, Dr. Rennebohm suggests that SuS should be considered in the differential diagnosis of any patient who presents with one or more of the following unexplained signs and symptoms:
“In general, SuS is treatable and responds to aggressive immunosuppression with corticosteroids, intravenous (IV) immunoglobulin and an immunomodulator such as mycophenolate or cyclophosphamide,” he reports.
Advertisement
In a recent Letter to the Editor published in the Journal of Neurological Sciences, Dr. Rennebohm and his colleagues present a case of a 52-year-old man who developed scotoma in his right eye, and one week later was admitted to the hospital with confusion, irritability, disinhibition, deafness in his left ear, vertigo, constipation and urinary incontinence.
The patient was diagnosed with SuS based on his symptoms and MRI results, and prescribed immunosuppressive therapy. He improved, but was readmitted to the hospital a month later with confusion, irritability, abdominal pain and intestinal hemorrhaging. He had no signs of cardiac involvement. He went on to go into hypovolemic shock, which necessitated a total colectomy. He was discharged with azathioprine and steroids and had two subclinical relapses necessitating IV steroids and maintenance therapy with mycophenolate mofetil before recovering.
“Although SuS primarily affects the brain, retina and inner ear, it’s possible that sometimes it will affect other organs, including muscle or the GI tract as we observed with this man,” says Dr. Rennebohm. “Although we need to see more cases before conclusions can be drawn, the purpose of the Letter to the Editor is to alert physicians to the possibly that SuS patients they are managing who also have GI issues could possibly have SuS-related microvasculopathy in their GI tract that warrants escalation of immunosuppressive therapy.” Alternatively, he notes, patients may develop GI infections or colitis as a result of the aggressive immunosuppressive therapy prescribed to manage SuS.
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications