A Q&A with Seth Rotz, MD

Advances in cancer treatment in the U.S. have led to a greater than 80 percent five-year survivorship rate for people diagnosed under the age of 20 — a substantial improvement from 30 years ago. While the progress is encouraging, it also demands we turn our attention to the growing population of pediatric cancer survivors at risk of late effects from the disease or its treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Seth Rotz, MD, Director of the High-Five Cancer Survivor’s Clinic at Cleveland Clinic Children’s, provides some insight into the changing landscape of pediatric cancer survivorship.
Q: What does cancer survivorship care look like today?
A: Of the more than 400,000 pediatric cancer survivors in the U.S., an estimated 73 percent will have a chronic health condition. Studies suggest 42 percent of those will likely experience a severe, disabling or life-threatening condition or death. Modifications in treatment are reducing exposures to radiotherapy and chemotherapy — especially for children as they tend to do better with the therapies. But we still need to increase efforts to detect and treat late effects as early as possible.
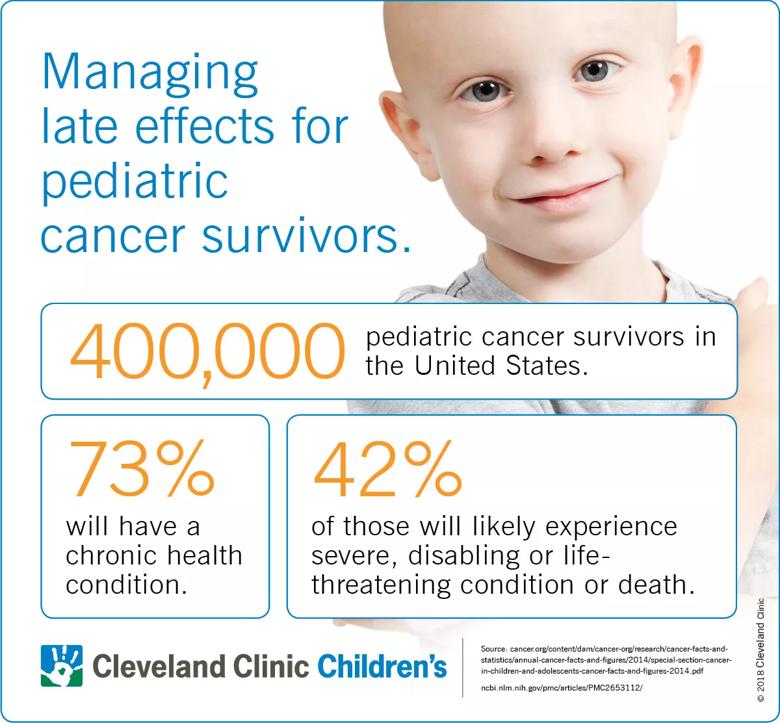
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7f1dc45e-5a33-4293-8d05-890e372b8934/18-CHP-124-QD-Cancer-Survivorship-1_jpg)
Generally, survivorship care begins five years after diagnosis. Care plans are designed to be holistic and integrated in their approach, allowing the survivorship medical team to orchestrate all aspects of patient’s follow-up care. While plans are customized to the surviving cancer patient, they typically include some combination of specialized education, screenings for long-term effects of chemotherapy and radiation, blood tests to look at hormone issues and kidney function, echocardiograms to look at potential weakening of the heart, pulmonary function testing, colonoscopies, mammograms, hearing examinations, neurological exams, nutritional counseling and more. Patients typically are seen annually, but may be seen more or less frequently, depending on need.
Advertisement
Q: Why is specialized care important for pediatric cancer survivors?
A: The critical aspect of this specialized care is early detection of long-term problems. Medical staff trained in cancer survivorship consider and respond to the type and location of a patient’s cancer, the type of treatments received, the age at diagnosis, other cancers or illness, patient history, and a host of other factors when treating patients or designing protocols for a patient’s primary care physician. Early incorporation and monitoring of lifestyle modifications and medications have shown to significantly reduce or prevent many late effects.
Important to consider, also, is that only 2 percent of all cancers is diagnosed during childhood, making pediatric cancer survivorship a very specialized field. Add to that, guidelines are constantly changing. The focus of a dedicated survivorship team ensures the best patient outcomes for childhood cancer patients.
Q: Can you provide some specific examples of late effects you’ve seen in pediatric cancer survivors?
A: A multitude of issues can develop in a person’s organs, tissues, joints, bones, body function, thinking, memory, and social and psychological development. Survivors also are at risk of secondary cancers and may have fertility and family planning concerns. This is why survivors need regular medical follow-up examinations to identify, monitor, and treat late effects appropriately.
Q: What recent research supports the need for pediatric cancer survivorship clinics?
Advertisement
A: Numerous studies and ongoing trials conducted by Cleveland Clinic and other medical research teams reinforce the need for survivorship education, treatment protocols and intervention strategies. Perhaps, most notably, the Childhood Cancer Survivor Study, funded by the National Cancer Institute in collaboration with other organizations, concluded pediatric cancer survivors were at a three times greater risk of developing a chronic condition and eight times greater risk of having a severe or life threatening condition than a sibling group.
Q: What is recommended to patients and families who want to move on and away from their experience with cancer?
A: Treatment always is the patient’s choice, but we highly encourage at least one follow-up visit — even a virtual visit — to ensure patients and their families make informed decisions about ongoing care. We find re-education to be especially important when patients are diagnosed and treated at very young ages, as caregivers tend to be consumed with emotion and distracted during the cancer diagnosis and initial therapy.
Q: Tell me more about the High-Five Cancer Survivor Clinic.
A: The High-Five Cancer Survivor’s Clinic at Cleveland Clinic Children’s is a long-term follow-up clinic for children and adults who have reached the point of five years from a diagnosis of cancer and who have been off therapy for at least two years. We are somewhat unique in that we have the credentials and experience to treat survivors into their adult years. As an internist, as well as a pediatric oncologist/hematologist, I technically can see patients into their 100s.
Advertisement
Advertisement

Findings hold lessons for future pandemics

One pediatric urologist’s quest to improve the status quo

Overcoming barriers to implementing clinical trials

Interim results of RUBY study also indicate improved physical function and quality of life

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

The benefits of this emerging surgical technology

Integrated care model reduces length of stay, improves outpatient pain management

A closer look at the impact on procedures and patient outcomes