An OB-GYN infectious disease specialist provides insight
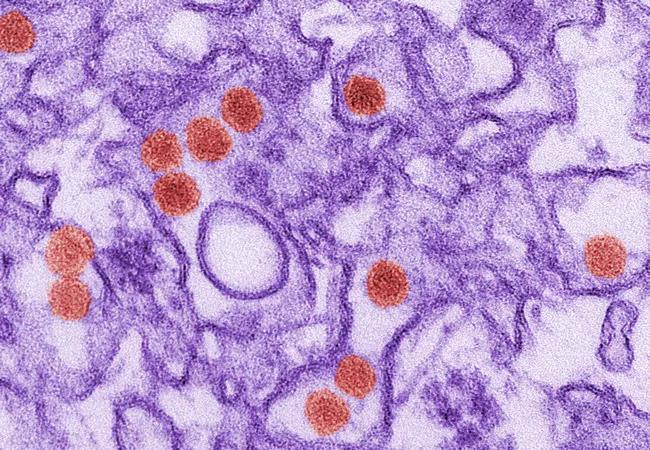

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/80760d7e-655a-4a28-9bb3-19d97404cfe0/Goje_Oluwatosin_150x180_jpg)
Oluwatosin Goje, MD, MSCR
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The Zika virus was first identified in Uganda in 1947, but until recently it has attracted very little media attention compared to its cousins in the flavivirus family, including the dengue virus and chikungunya virus.
That changed in 2015, when Brazil witnessed a 20-fold increase in the number of babies born with microcephaly, some of whom were infected with the virus.
While countries with reported active Zika transmission remain primarily in South America, Central America and the Caribbean islands, it’s difficult to determine how the virus will spread over time.
As of Feb. 10, 2016, the Centers for Disease Control and Prevention (CDC) reported 52 travel-associated Zika virus disease cases in the United States. Although the number is small, U.S. primary care physicians should take note, says Oluwatosin Goje, MD, MSCR a Cleveland Clinic specialist in reproductive infectious disease. She cites two primary reasons for concern.
“The world is a global village. A lot of people travel outside the country for vacation and work who could come back with an infection,” says Dr. Goje. “Second, we have Aedes mosquitos in this country that are native to us.” The CDC has predicted that travelers would occasionally bring Zika to the U.S., but said any further spread would be very limited because the Aedes aegypti mosquito that carries the virus is restricted to warm areas in the extreme south, such as south Texas, south Florida and Hawaii.
The primary mode of transmission is from the Aedes species of mosquitoes. “They bite an infected person and take the virus into their system,” says Dr. Goje. “When they bite somebody else, they transmit the virus they have acquired into that next person.” Aedes mosquitoes, including Aedes aegypti and Aedes albopictus, usually lay eggs in and near standing water and are aggressive daytime biters, according to the CDC.
Advertisement
Maternal-fetal virus transmission, either intrauterine or perinatal, is also possible. In addition, the Zika virus may be passed on sexually, through a blood transfusion or laboratory exposure. The CDC notes that Zika virus RNA has been identified in asymptomatic blood donors during an ongoing outbreak.
Dr. Goje says most patients with zika virus infection will be asymptomatic. The infection rate is 73 percent, yet the symptomatic attack rate among the infected is just 18 percent. “So only one out of five people will be symptomatic,” says Dr. Goje. “The majority of people will feel normal after contact.” In addition, the symptoms for that 18 percent are non-specific as listed below and often mild, says Dr. Goje.
Characteristic clinical findings include the following:
Symptoms last several days to a week and typically don’t require hospitalization. “Most people may not even talk to their primary care physician,” says Dr. Goje. “They often take a mild analgesic and shake it off.”
However, she cautions that the recent rise in cases and spread of the Zika virus should prompt heightened awareness in patients and physicians. “If anyone has traveled to a Zika-affected area and remembers having a rash, fever, joint pain, pink eye or headache within two weeks of coming home, they need to reach out to their doctors,” she says.
There aren’t any commercially available diagnostic tests for Zika virus diseases. Testing is performed at the CDC Arbovirus Diagnostic Laboratory, and a few state and local health departments. Diagnostic testing includes:
Advertisement
Anyone suspected of having Zika virus disease should also be evaluated for possible dengue or chikungunya virus infections because of similarities in geographic distribution and symptoms.
There is no antiviral therapy or vaccine for those infected with Zika virus disease. Supportive treatment is generally recommended, including rest, fluids and the use of analgesics and antipyretics. Avoid aspirin and other non-steroidal anti-inflammatory drugs until the possibility of dengue is eliminated to decrease the risk of hemorrhage.
In early February, the World Health Organization declared Zika a public health emergency of international concern. Research into the Zika virus is ongoing, but much remains unknown. Dr. Goje cites three research areas that primary care physicians should keep abreast of:
In the meantime, pregnant women with a history of travel to an area with ongoing Zika virus transmission should follow CDC guidelines and be tested for the infection. Those with positive or inconclusive results should consider a series of fetal ultrasounds and amniocentesis for Zika virus testing. Those who test negative for the virus should still consider a fetal ultrasound to detect microcephaly or intracranial calcifications.
Advertisement
With reports on the Zika virus inundating the 24-hour news cycle, it’s important to put the virus in perspective. Dr. Goje has three takeaway points for primary care physicians.
The first is to remember that Zika is not contagious, so we do not need to isolate patients. “I don’t want people to get panicked and go into a frenzy,” she says. “This is not contagious.”
Second, Dr. Goje would like physicians to remind patients that the CDC recommendation for pregnant women to avoid travel to Zika-affected areas is not because of a doomsday scenario. “It’s a precautionary measure while so much research is still going on,” she says. “It’s safer to stay at home while researchers figure out what is going on.”
Dr. Goje’s third piece of advice is for physicians to ask all pregnant patients about their travel plans. If they intend to visit a Zika-affected area and can’t postpone travel, then they need to understand some preventive measures:
Despite its newsworthiness, a lot of mystery still surrounds the Zika virus. While researchers learn more about the virus and infection, both physicians and patients should err on the side of caution, concludes Dr. Goje. To stay up-to-date on the Zika virus, visit the CDC website.
Advertisement
Advertisement

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity

Psychological care can be a crucial component of medical treatment