Pushing the envelope in musculoskeletal oncology care

By Nathan W. Mesko, MD; Lukas M. Nystrom, MD; Jacob G. Scott, MD, DPhil; Scott Kilpatrick, MD; and Amanda Maggiotto, MBA
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The words “tumor,” “lesion” and“mass” elicit a flood of emotions for patients receiving a new diagnosis. Though the vast majority of new bone and soft tissue lesions are benign, having an abnormal finding is nerve-racking for patients. As a patient-focused Musculoskeletal Tumor Center, we have made reducing this anxiety a top priority through protocols that expedite treatment or time-to-treatment initiation (TTI). We define TTI as the time from diagnosis to treatment.
In this article we review techniques and processes that are decreasing our TTI in meaningful ways – and improving patient care (Table 1).
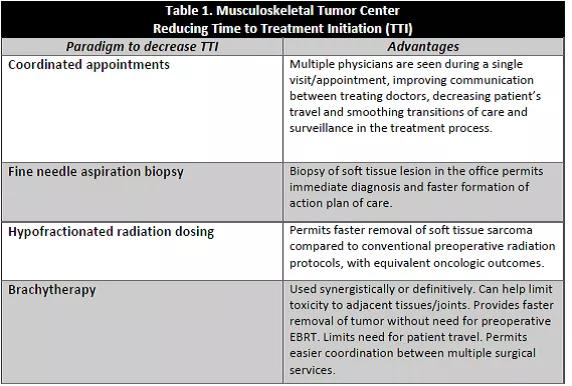
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1daab533-ea06-4745-b899-97e9f12f2656/meskoTable1_png)
Coordinated care visits and multidisciplinary clinic model. Multiple physicians are involved in treating patients with bone or soft tissue sarcoma, metastatic disease involving the musculoskeletal system and certain aggressive benign tumors. Our goal is for patients to have all pertinent initial appointments completed in a single visit, which also gives us the ability to begin planning for treatment the same day a diagnosis is made.
A multidisciplinary clinic model trims excess time — sometimes by days or weeks — that would otherwise delay the start of treatment.
Fine needle aspiration combined with core needle biopsy. Combining core needle biopsy and fine needle aspiration (FNA) as part of the initial office-based biopsy protocol may help reduce TTI.
While core needle biopsy has the advantage of obtaining a large amount of tissue for diagnostic purposes, it can take three to five days for final diagnosis to be reported due to tissue processing requirements. Instead, we employ FNA in conjunction with a core needle biopsy in the office setting for masses that are palpable and do not require image targeting.
Advertisement
By including FNA along with core needle biopsy, our soft tissue pathology team can often provide a preliminary diagnosis within minutes after the biopsy. Having this early information allows us to begin any additional evaluations that may be required, and begin discussing preliminary information and testing with patients prior to them leaving the office. Having this preliminary diagnosis also helps us move treatment planning forward more rapidly (Figure 1).
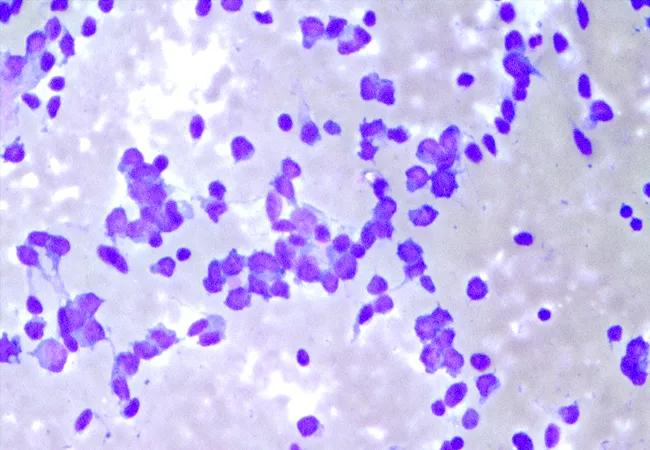
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e4e8b70a-26de-4bf2-af81-d3423ec14705/18-ORT-1149-Mesko-Inset-02_jpg)
Figure 1. Fine needle aspirate of synovial sarcoma on air dried Diff-Quik® stain (above) for immediate interpretation, and Papanicolaou alcohol-fixed smears for later review (below).
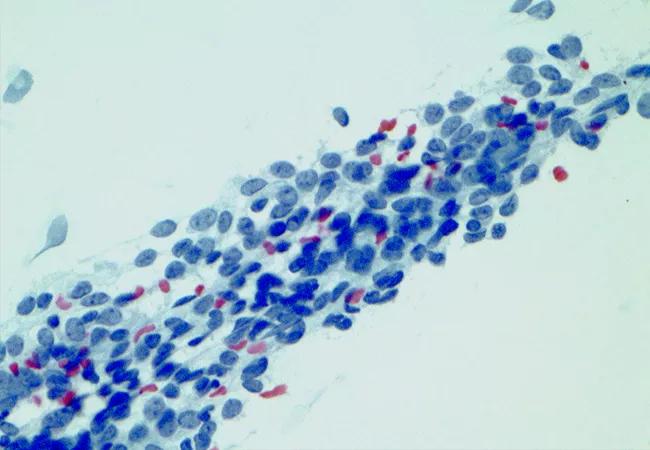
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/12a6949c-6821-4bcd-ab94-96846f5aae60/18-ORT-1149-Mesko-Inset-03-650x450pxl_jpg)
Hypofractionated preoperative radiation. Surgery in combination with radiation decreases risk for local recurrence of soft tissue sarcomas. Traditionally, preoperative radiation therapy takes place over the course of five weeks, with an additional three to six weeks of rest for radiation skin effects to heal prior to surgery. In other words, a patient could wait two to three months between diagnosis and surgery.
Cleveland Clinic uses a new protocol that reduces this time period significantly. Hypofractionated preoperative radiation condenses the traditional five weeks of radiation into five days with biologically equivalent results. In addition, rather than following the traditional three- to six-week rest period, we now remove the sarcoma definitively within 12 to 72 hours after radiation ends.
Recent studies1 demonstrate that hypofractionated preoperative radiation yields similar local recurrence rates and lowers early and late complications compared to traditional radiation dosing.
Advertisement
Many patients travel significant distances to our tertiary sarcoma center for treatment. This new radiation therapy approach makes treatment much more convenient for patients and allows us to continue providing gold-standard treatment for this rare cancer.
Brachytherapy (interstitial catheter-based radiation). Brachytherapy, used either with traditional external beam radiation (EBRT) or as definitive treatment, continues to be of great value in select soft tissue sarcoma cases.
Synergistic effects with EBRT — Traditional beam radiation can be toxic to adjacent organs, tissue and bone/joints. Brachytherapy, on the other hand, can limit the overall dose of radiation to adjacent tissue without sacrificing dose to the tumor bed. We often deliver a low preoperative dose of EBRT to areas where toxicity from radiation can lead to potentially difficult long-term sequelae (joint stiffness, mucosal surface irritation, wound healing difficulties, etc.).
Sarcoma surgeons resect the tumor, then implant brachytherapy catheters. Postoperatively, additional radiation can be delivered in an even more localized fashion through the catheters, limiting toxic level dosing to adjacent tissues.
Brachytherapy as definitive treatment – By utilizing brachytherapy as definitive treatment, we can forego preoperative radiation and instead remove the tumor shortly after diagnosis. Catheters are implanted at the time of surgery, and radiation is completed while the patient is in the hospital. The patient returns to the operating room for catheter removal and final soft tissue reconstruction, usually within five to 10 days. In addition to earlier tumor resection, this technique obviates the need for patients to return daily for radiation therapy. Furthermore, use of brachytherapy can simplify wound reconstruction in combination with plastic surgery. Reconstruction is scheduled at the completion of brachytherapy, when surgical margins are confirmed and the plastic surgeon has prepared for the known soft tissue defect and planned reconstructive options (Figures 2 and 3).
Advertisement
Whether meeting a patient for the first time with a new radiographic or clinical exam findings, seeing patients for their five-year follow-up visit, providing a second opinion consultation, or walking a patient with an active cancer diagnosis through a difficult journey, we recognize the opportunity to build relationships with our patients that can create a powerful treatment team. We are committed to adapting our practices to meld evidence-based medicine and patient needs to produce the best possible oncologic and functional outcomes.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a1b907fd-ef9e-416f-81bb-f08f2aa8cfc5/18-ORT-1149-Mesko-Inset-01-650x450pxl_jpg)
Figure 2. A 53-year-old male with poorly controlled blood sugars presented with a one-month history of an enlarging thigh mass, biopsy proven as a high-grade myxofibrosarcoma involving the sartorius muscle. One week after diagnosis, we performed a wide en bloc excision. Immediately after excision, brachycatheters were placed in the wound 1 cm apart to cover the entire resection bed. White foam was placed over the femoral vessels and nerve structures, which were protected from the tumor by the adjacent resected sartorius muscle.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b7a9b5f8-c887-47fc-82ac-877c34ddba6d/18-ORT-1149-Mesko-Hero-Image-650x450pxl_jpg)
Figure 3. Once the catheters were placed and anchored to the tissue, a negative pressure device utilizing black foam was placed to cover the catheters. The patient then underwent five days (nine fractions, 38Gy) of radiation treatments while admitted to the hospital. He underwent definitive plastic surgery reconstruction one week after the en bloc excision, once margins were determined clean. Brachytherapy was considered definitive treatment in this case.
Advertisement
Reference
Drs. Mesko and Nystrom are orthopaedic oncologists, and Dr. Mesko directs the Musculoskeletal Tumor Center. Dr. Scott, Department of Radiation Oncology, specializes in sarcoma radiation. His laboratory focuses on Ewings sarcoma and cancer evolution using mathematical modeling, data science and experimental evolution. Dr. Kilpatrick, Department of Pathology, has special interest in bone and soft tissue tumors. Ms. Maggiotto is Sarcoma Program Manager.
Advertisement

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units