Outcomes research explores antibiotic regimens
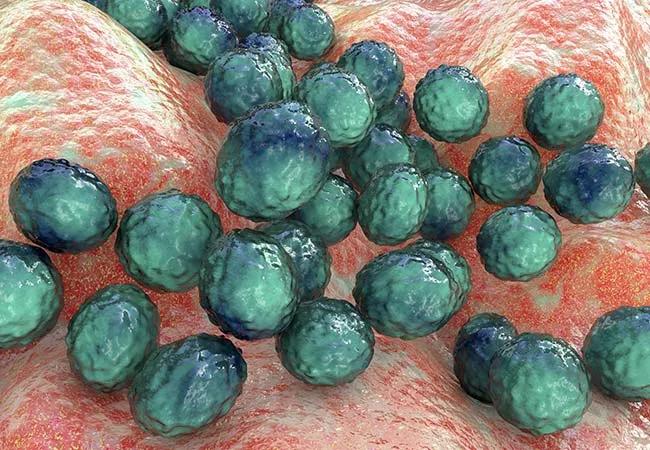
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5b9329dc-0090-435b-914b-60d28b06e342/21-CHP-2393663-Hero-650x450-1_jpg)
21-CHP-2393663-Hero-650×450
Staphylococcal scalded skin syndrome (SSSS) is an exfoliative dermatitis mediated by Staphylococcus aureus toxin, and its incidence is rising. A prior study demonstrated variability in the evaluation of children with SSSS, but the degree of testing did not impact patient outcomes.1
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The treatment of SSSS includes both supportive measures and antistaphylococcal antibiotics. Clindamycin has historically been included in treatment to inhibit bacterial protein synthesis.2 However, a paucity of data raises questions about the most effective antibiotic(s) for SSSS. Is clindamycin monotherapy sufficient, or are additional antibiotics more effective?
A multi-institution team, including Dana Foradori, MD, a pediatric hospitalist at Cleveland Clinic Children’s, utilized the Pediatric Health Information System database to review outcomes among children admitted to U.S. children’s hospitals with SSSS from 2011-2016.3
The most frequently utilized antibiotic regimens were clindamycin monotherapy, clindamycin + methicillin-resistant S. aureus coverage and clindamycin + methicillin-sensitive S. aureus coverage.* In patients who received these regimens, we did not find any associated differences in length of stay or treatment failure, even after adjustment for illness severity. Combination therapy was associated with higher cost in this population.
Prospective trials are necessary to confirm these findings, especially in light of evolving S. aureus resistance.
*Additional antibiotic regimens, including MSSA and MRSA-directed monotherapy, were infrequently utilized, and sample size was insufficient for analysis.
References
Advertisement
Advertisement
Findings hold lessons for future pandemics
One pediatric urologist’s quest to improve the status quo
Overcoming barriers to implementing clinical trials
Interim results of RUBY study also indicate improved physical function and quality of life
Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner
The benefits of this emerging surgical technology
Integrated care model reduces length of stay, improves outpatient pain management
A closer look at the impact on procedures and patient outcomes