Why enhancing clinical care is critical for patient outcomes

Hematopoietic stem cell transplantation (HSCT) requires a prolonged hospitalization and patients often face an increased risk of complications, including transplant-related mortality. And so, enhancing clinical care and identifying best practices is critical for patient outcomes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Over the last couple of years, we have been working to develop a learning network for transplant patients (TALNT),” says Seth Rotz, MD, Pediatric Hematology Oncology and Blood and Marrow Transplantation, Cleveland Clinic. “The goal of this initiative is to build a resource that allows us to learn from one another’s best practices, track data, and work as a group to identify ways to improve care for these patients.”
As a part of this ongoing effort, Dr. Rotz and colleagues sought to help the clinical community better understand quality improvement and how it pertains to bone marrow transplant patients. In a recently published review paper, this multi-institutional team of experts explored the importance of quality improvement and made the case for using The Model for Improvement framework (Transplant Cell Ther. 2022;28(5):233-41).
“Bone marrow transplant patients are among the most complex group in the hospital. All of them have multiple issues and there are multiple sub-specialists involved,” notes Dr. Rotz. “Therefore, the problems we encounter are often multi-dimensional and aren’t just solved by conducting a trial of A or B. We are contending with dynamic issues and often to fix them it helps to have a quality improvement mindset as opposed to a clinical trial mindset.”
When asked to discuss the key takeaways from their review paper, Dr. Rotz emphasized the importance of distinguishing between quality improvement and quality assurance—two related yet distinct concepts. “There is a difference between quality improvement and quality assurance, and I believe this is often misconstrued in the healthcare setting,” he notes.
Advertisement
“Quality improvement applies a systematic, multidisciplinary approach to improving patient safety, experience, and effectiveness in healthcare delivery,” Dr. Rotz and colleagues explain. “Quality improvement is an active process of designing, testing, and implementing changes to the healthcare delivery system to improve the process or outcome measures.”
In comparison, quality assurance reviews “compliance against specific standards to minimize gaps between policy and practice.” When it comes to the HSCT setting, this is primarily accomplished through the Foundation for the Accreditation of Cellular Therapy (FACT) and Joint Accreditation Committee ISCT-Europe & EBMT (JACIE).
Both quality improvement and quality assurance have important roles to play in healthcare, and more specifically HSCT, emphasizes Dr. Rotz. When HSCT standards are not met, quality improvement methods are used. This includes creating a specific aim, identification of key drivers, and measurement of the outcome. It’s use, however, is not limited to this, according to the review authors, who noted that quality improvement should be used continuously to improve outcomes among this population.
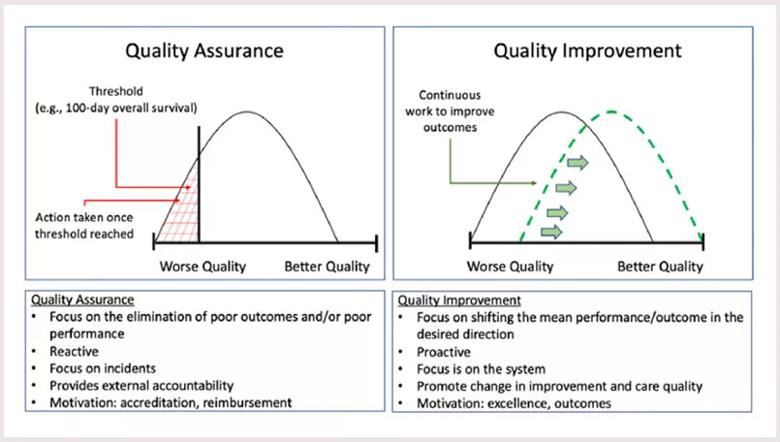
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/057354f1-f9d2-451f-aa33-2aa58c5b2b08/22-CHP-2999112-CQD-Rotz-Qual-Improve-in-Hematopoietic-inset_jpg)
Figure 1. QA versus QI: The focus of QA is to eliminate poor outcomes/performance, whereas QI attempts to shift an entire outcome curve toward a defined aim. Image reproduced with permission from Elsevier. Originally published: Transplant Cell Ther. 2022 May;28(5):233-241.
There are various quality improvement models, but in their review Dr. Rotz and colleagues argue for the use of The Model for Improvement —“a powerful tool for accelerating continuous healthcare improvement.”
Advertisement
This model, they note, has been used successfully implemented by hundreds of healthcare organizations across multiple countries to improve different processes and outcomes. When using this model, teams are asked three key questions:
The Model for Improvement, which uses a rapid process (PDSA cycles) to develop, test, implement, and improve patient safety and healthcare delivery quality, is a “robust quality improvement tool that transplantation and cellular therapy teams can use to redesign healthcare processes to improve patient care,” suggest Dr. Rotz and colleagues.
A frequent challenge in the HSCT setting is that healthcare systems and administration tend to put an emphasis on quality assurance rather than quality improvement, according to Dr. Rotz, who notes that there is often a punitive connotation associated with not hitting benchmarks.
“Quality improvement on the other hand focuses on moving the system as a whole forward,” he says. “By using The Model for Improvement we have the opportunity to make outcomes for a challenging group of patients better. This approach allows us to address issues that aren’t classically thought of when we’re considering outcomes for patients, such as quality of life and length of hospital stay.”
Focusing on quality improvement also holds value when it comes to implementation. “We already have a strong understanding of what is important to these patients and what works, but we sometimes struggle as a system with the complexities of implementation,” says Dr. Rotz, who gave the example of the bone marrow transplant patient with a fever.
Advertisement
“We know they should receive antibiotic within an hour in case they have a bloodstream infection. However, there are a number of system-based issues that may make this challenging,” he notes. “Through quality improvement methods we have the opportunity to solve complex, inter-related problems that directly affect outcomes for our patients.”
Advertisement
Advertisement

Findings hold lessons for future pandemics

One pediatric urologist’s quest to improve the status quo

Overcoming barriers to implementing clinical trials

Interim results of RUBY study also indicate improved physical function and quality of life

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

The benefits of this emerging surgical technology

Integrated care model reduces length of stay, improves outpatient pain management

A closer look at the impact on procedures and patient outcomes