Vaccines, testing and patient education are needed

Editor’s Note: In November 2022, the World Health Organization and the U.S. Centers for Disease Control and Prevention renamed the monkeypox virus “mpox.” We have updated some language in this article to reflect that change (although not in contemporaneous quotes or references to previously conducted studies), and will use mpox in new articles relating to the virus.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The mpx virus has little in common with SARS-CoV-2, but the 2022 global mpx outbreak nonetheless raises questions reminiscent of the early months of the COVID-19 pandemic: Should we be more worried than we are, and if so, what should clinicians be doing about it?
Steven Gordon, MD, Chairman of Infection Disease at Cleveland Clinic, says the mpx outbreak – some are calling it a pandemic – is cause for concern. There’s still a lot to know about the spread, and it is taxing a public health system already fatigued from more than two years of COVID-19. “We’re still not through with one pandemic, and now we have a new emerging zoonotic virus,” Dr. Gordon says.
As of July 28, 2022, more than 20,600 cases had been identified worldwide. With more than 4,600 known cases confirmed in the United States, the U.S. is one of 71 affected countries where mpx is not endemic.
Many more undiagnosed cases are presumed to exist, although how many remains a question. Five commercial laboratories in the U.S. have begun ramping up their testing capacity for mpx, but testing has so far been limited.
Common mpx symptoms include fever, headache and body aches, and an itchy or painful rash that can develop on the face and inside the mouth, and on hands, feet, chest, genitals and anus. A typical case will have a febrile prodrome 5-13 days after exposure followed 1-4 days later with onset of a characteristic deep-seated vesicular rash with a centrifugal (moving from hands and face to trunk) distribution. The lesions are usually well circumscribed and often umbilicate, progressing over time to scabs. There is usually associated swelling of the local lymph nodes.
Advertisement
Transmission is through close, sustained physical or sexual contact with someone who has monkeypox, or through contact with objects, such as bedsheets, that contain fluids from someone with symptoms. Anyone can become infected, but the 2022 outbreak has been prevailingly found in men who have sex with men, people who are gay or bisexual, and those who are in close physical contact with them.
“The last outbreak of monkeypox in the U.S. was in 2003 and was associated with exposure to infected animals (prairie dogs) without person-to-person transmission,” Dr. Gordon says. “Sexual transmission has been described in the past, but appears to be the predominant mode of transmission in the cases reported so far. We do not know whether the virus may spread through contact with semen or vaginal fluids, or the role of aysmptomatic transmission.”
Unlike COVID-19, which has killed more than 6.3 million worldwide, mpx infection usually does not require hospitalizations or result in death.
The Centers for Disease Control and Prevention reports that cases from the 2022 outbreak are of the West African type, which has a survivability rate of more than 99%. (The Congo Basin clade has about a 10% fatality rate.)

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b2b9fc08-a20b-4060-9b9e-1c6b87098251/22-CCC-3109762-CQD-Inset1-800x800-2_jpg)
Initial macule development

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/be4c98ce-cd46-4e32-968f-2048431c5be5/22-CCC-3109762-CQD-Inset2-1_jpg)
Rash becomes papular

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e2b98f52-d3a9-441f-ac92-1fb1a6ec653e/22-CCC-3109762-CQD-Inset3_jpg)
Vesicles develop

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/aab1caf0-c434-41c1-bbd0-c0bb3b6b0354/22-CCC-3109762-CQD-Inset4_jpg)
Pustules form

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2113c436-f906-499c-9312-f5b84683f5bf/22-CCC-3109762-CQD-Inset5_jpg)
Scabs form
Physicians and nurses who work in sexual health clinics and urgent care centers are likely to occupy the first line of defense, Dr. Gordon says. Messages to patients should be similar to those that have been counseled for years in the HIV and sexually transmitted infections space: practice safe sex. “Some antivirals can be used for treatment of monkeypox, but mostly we’re going to contain the outbreak with pre-exposure prophylaxis vaccination for patients who are known contacts or at highest risk for acquisition,” Dr. Gordon says.
Advertisement
“I’m a big advocate of doing what is being done in New York in Los Angeles, and setting up clinics for targeting the same population to whom we would give Truvada®,” adds Dr. Gordon. “People want to protect themselves, and as the transmission continues in communities, vaccination is a strategy for prevention. The major challenge to date is vaccine supply.”
Since May, U.S. Health & Human Services has made about 300,000 doses of Bavarian Nordic’s JYNNEOS vaccine available to states for distribution. More has been ordered, but in New York and California, where demand has been highest, supplies are still lagging.
By mid-July in Ohio, Dr. Gordon says, fewer than 10 vaccines had been given. But he expects to see that grow as risk awareness expands and more cases are diagnosed locally, and believes PreP clinics should be used here as well.
“If you ring the bell, people might think it’s ridiculous: Why would you open up these clinics in Ohio? We only have eight cases diagnosed,” he says. “But that is likely a lagging indicator of the true number of cases. Each day is a new opportunity for transmission. It’s better to have vaccines with no virus than virus with no vaccines.”
In the meantime, he says, healthcare providers should counsel patients, especially those in high risk categories, to protect themselves against exposure. The CDC recommends frequent hand washing with soap and water or sanitizer, and to avoid:
Advertisement
Advertisement

Advanced software streamlines charting, supports deeper patient connections

How holding simulations in clinical settings can improve workflow and identify latent operational threats

Interactive Zen Quest experience helps promote relaxing behaviors

Cleveland Clinic and IBM leaders share insights, concerns, optimism about impacts
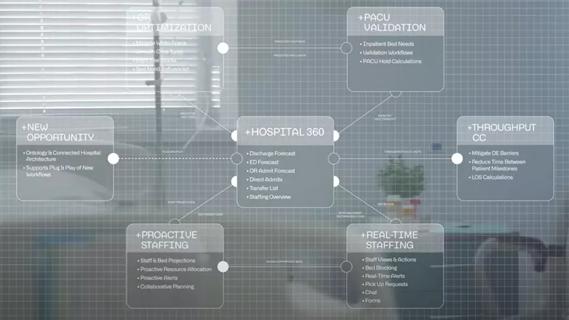
Cleveland Clinic partners with Palantir to create logistical command center

A Q&A with organizational development researcher Gina Thoebes

Cleveland Clinic transformation leader led development of benchmarking tool with NAHQ

Raed Dweik, MD, on change management and the importance of communication