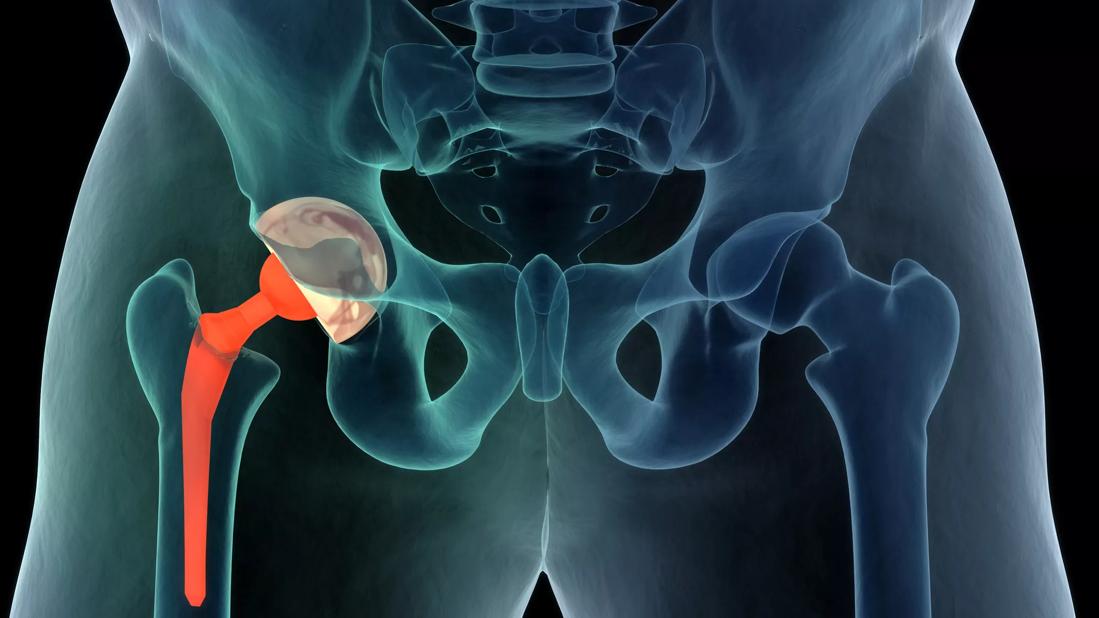
Total joint arthroplasties (TJA) are among the most common of elective surgeries. According to the American Academy of Orthopaedic Surgeons, nearly 2 million hips and knees will be replaced annually in the United States by 2030, to say nothing of shoulders, elbows, wrists, and ankles.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The projected growth in these surgeries means a corresponding increase in periprosthetic joint infections (PJIs), a leading cause of arthroplasty failure. With an average incidence of 70,000 cases per year, PJIs are projected to cost the U.S. healthcare system $2.2 billion annually. “Perhaps most concerning is the 5-year mortality rate of 26% among patients with joint infections, which is worse than many common cancers,” says Cleveland Clinic Florida orthopaedic surgeon Carlos Higuera-Rueda, MD, FAAOS.
A past president of the Musculoskeletal Infection Society (2019), Dr. Higuera is Chairman of the Levitetz Department of Orthopaedic Surgery for Cleveland Clinic Weston Hospital and Center Director for Orthopaedic and Rheumatology. As a leading researcher in PJI, much of his work is focused on developing better diagnostic tools and infection prevention and treatment techniques and protocols.
He participated in the 2022 American Association of Hip and Knee Surgeons (AAHKS) Annual Meeting Symposium on Periprosthetic Joint Infection and co-authored a symposium summary published earlier this year that provides an overview of current techniques in PJI prevention, diagnosis, and management.
Consult QD had the opportunity to talk with Dr. Higuera about some of the latest developments in the field, including many PJI research initiatives underway at Cleveland Clinic. Here are the big takeaways.
What’s In
- Risk calculators and predictive modeling:
In the area of prevention, several initiatives are underway to develop risk calculators and predictive modeling tools to help patients approach joint arthroplasty with their eyes wide open and aid clinicians in preoperative counseling and clinical decision making. Dr. Higuera points to the NarxCare score (NCS), which identifies risky drug-use patterns, as a useful tool to guide a patient-centered discussion regarding possible postoperative risks associated with prescription drug-use. In another example, he cites a retrospective study by a team of researchers using machine learning as a tool for PJI prediction following revision total knee arthroplasty (TKA) for patients with aseptic indications for revision surgery. - Point-of-care testing:
The diagnosis of PJI remains challenging despite the availability of a variety of tests. According to Dr. Higuera, one important tool missing from the diagnostic toolbox is an effective “ruling out” test, though he is optimistic one is on the horizon. He and his Cleveland Clinic colleagues in Florida and Ohio published a prospective cohort study that tested the value of a point of care synovial calprotectin test for PJI diagnosis in patients undergoing TKA. Calprotectin is a protein biomarker that displays antimicrobial protective properties and is currently used in the management of patients with inflammatory bowel disease. “The calprotectin POC test demonstrated near perfect accuracy in the diagnosis of PJI, including high sensitivity and specificity,” says Dr. Higuera. - Next-generation sequencing:
While conventional cultures of joint aspirate and intraoperative tissue samples are a mainstay in PJI diagnosis, the rise in culture-negative PJI has spurred research into other methods of pathogen identification, including next-generation sequencing (NGS). Cleveland Clinic was one of 14 centers participating in a multicenter study that used NGS to identify pathogenic organisms in approximately two-thirds of culture-negative PJIs tested. “The majority of infections were determined to be polymicrobial,” notes Dr. Higuera, a study co-author. - Aggressive antimicrobial treatments:
Bacterial biofilms on implants protect pathogens from antibiotics and the body’s immune response. Because they are also resistant to mechanical removal methods, such as brushing and scrubbing, biofilm eradication currently requires implant removal and replacement. Dr. Higuera is part of a team of researchers who have developed a new antimicrobial treatment successfully tested in an animal model for eradicating mature Staphylococcus aureus biofilms grown on 3D-printed Ti-6Al-4V alloy implants.
According to the 2023 study in ACS Applied Bio Materials, the two-step approach uses a near-infrared light-activated hydrogel nanocomposite system for thermal treatment, following initial disruption with d-amino acids (d-AAs). They are delivered to the infection site as a solution that transforms to a gel state at physiological temperature. “Our goal is to eradicate biofilms without replacing implants. We are still in the early phase of treatment development, but these initial results give me hope that a solution is possible,” says Dr. Higuera.
What’s Out
- Potent anticoagulation agents:
Persistent wound drainage, a known risk factor for PJI, can be exacerbated by aggressive anticoagulation agents. According to the authors of the PJI Symposium summary, research supports a more cautious approach to venous thromboembolism prevention in patients undergoing joint replacement. “Today we are more likely to choose aspirin over more potent anticoagulation agents that can result in major wound drainage,” confirms Dr. Higuera. - D-dimer for screening:
Despite being identified as a PJI biomarker in the 2018 International Consensus Meeting definition of PJI, Cleveland Clinic Florida researchers found serum D-Dimer to have poor accuracy in discriminating between septic and aseptic cases in the setting of revision hip and knee arthroplasty. More recently, the team expanded on their research, demonstrating that the biomarker performs poorly in the setting of both low-virulence and high-virulence infecting organisms. - Two-stage exchange arthroplasty:
Removal of an infected prosthesis is one of the methods used to manage chronic PJI. While two-stage revision is currently the preferred method among U.S. surgeons, a growing body of research points to one-stage revision as a better option in terms of lower mortality rates and better quality of life. “Patients with ample soft tissue and minimal bone loss whose infection is caused by an antibiotic-susceptible pathogen are more likely to benefit from a one-stage approach,” says Dr. Higuera.