Advancements in technology and surgical techniques have broadened the use of sacral neuromodulation as a safe and efficacious management option for patients with fecal incontinence.
Sacral neuromodulation (SNM) has emerged as the leading surgical intervention for patients with fecal incontinence (FI) refractory to conservative measures. The condition affects up to 14% of U.S. adults over a lifetime and significantly impairs quality of life.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Many treatments have come and gone in the effort to help patients with fecal incontinence, but sacral neuromodulation has withstood the test of time,” says Emanuela Alvarenga, MD, FACS, FASCRS, a board-certified colorectal surgeon with Cleveland Clinic Tradition Hospital in Port St. Lucie, Florida. “The treatment has proven to be safe, effective and durable, and with continued advancement, it is helping more patients regain bowel control.”
SNM was first approved in the United States in 1997 for the treatment of urinary urgency incontinence and later expanded to idiopathic non-obstructive urinary retention. It received FDA-approval for fecal incontinence in 2011 and is now recommended as a first-line surgical option for incontinent patients with or without sphincter defects, per clinical practice guidelines issued in 2023 by the American Society of Colon and Rectal Surgeons.
Fecal incontinence, or accidental bowel leakage, has many causes including but not limited to:
“Fecal incontinence can be common in people with pelvic floor disorders, especially among female patients,” states Dr. Alvarenga. She estimates that approximately 10% of her overall practice and nearly 40% of the patients currently seen for pelvic floor dysfunction struggle with bowel control issues.
Advertisement
A retrospective cohort study published earlier this year in the American Journal of Gastroenterology also found that class II and III obesity are independently associated with a significantly higher risk of FI, with altered rectal sensitivity.
“Even everyday medications, like metformin and SSRIs, can cause motility changes that tip the balance toward incontinence,” explains Dr. Alvarenga. “That’s why a thorough history, exam and pelvic floor tests, including a colonoscopy to assess the health of the colon mucosa, are needed to zero in on the root causes and to develop individualized treatment plans.”
While many patients with FI benefit from first‐ and second‐line therapies, such as behavioral modifications, dietary adjustments, bulking agents, and antidiarrheal medications, a substantial subset remains symptomatic. For these individuals, SNM offers a minimally invasive, effective intervention.
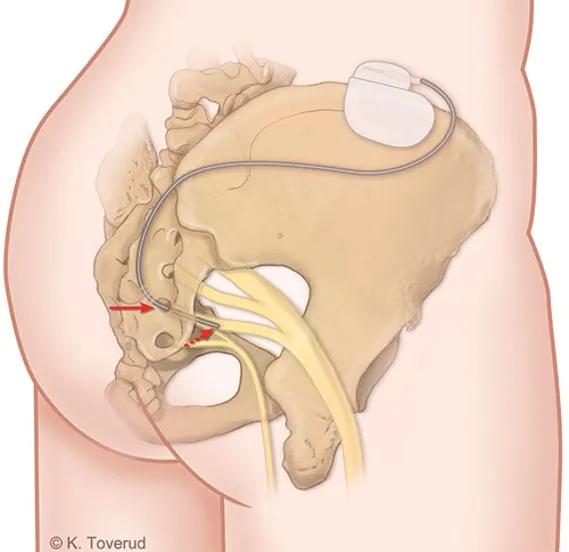
It works by gently stimulating the sacral nerves (predominantly S3) that coordinate the pelvic floor, rectum, and anal sphincter. Dr. Alvarenga notes that the exact mechanism at work is not fully understood but cites recent studies that suggest SNM may modulate aberrant signals between the sacral nerve roots and the central nervous system.
“In practice, sacral nerve stimulation improves the global function of the pelvis, reducing bowel accidents and improving quality of life,” she says. “Patients who also struggle with urinary incontinence may experience resolution of their urinary symptoms, as well.”
Advertisement
Candidates for SNM undergo an initial test phase prior to implantation. During an outpatient procedure, a thin lead is placed through the sacral foramen and then connected to an external pulse generator. Patients keep a bowel diary, tracking incontinence episodes and urgency over the brief trial period. If there is at least 50% improvement in symptoms, a permanent pulse generator will be implanted.
“The device is slightly larger than a quarter and is implanted just below the skin of the beltline in the gluteal region,” describes Dr. Alvarenga.
Studies have shown the trial-to-implant success rate hovers around 80%. Improvements in lead placement techniques have also increased surgical accuracy and greater therapeutic success.
The benefits of sacral neuromodulation have been demonstrated in patients with sphincter defects, following sphincter repair and with pudendal neuropathy, as well as in patients who have had rectal resections with neorectal reconstructions.
Technological refinements of SNM implants have broadened the use of sacral neuromodulation for bowel control. “The newer devices are smaller and lighter, with longer battery life lasting up to 15 years, rechargeable options, and MRI compatibility,” says Dr. Alvarenga.
The latest InterStim™ Micro device (2.8 cm³), for example, offers an 80% volume reduction versus the older InterStim™ II (14 cm³). MRI-compatibility also removes imaging contraindications, making it a treatment option for patients with FI who require periodic MRIs.
Advertisement
Though rechargeable systems promise a decade or more service, some patients still opt for fixed battery models to avoid frequent recharging, reports Dr. Alvarenga.
“Some of our slimmer patients prefer the smaller rechargeable devices to improve comfort, while some patients with higher BMI find charging the device more difficult,” she says. “The good news is that we have more options to suit a patient’s individual needs.”
Despite being a treatable condition that effects more than 21 million Americans, many people do not talk about fecal incontinence, even with their physician. One study estimated 70% of women with accidental bowel leakage do not seek care.
Dr. Alvarenga encourages primary care providers, gynecologists, urogynecologists and gastrointestinal specialists to ask their patients about symptoms of FI and to reassure them that treatments are available. She also recommends a low threshold for referring patients with fecal incontinence after conservative therapy fails.
“Even though many patients may not initially share their symptoms voluntarily, posing the question opens the door to seeking specialized care,” she says. “I find it very rewarding to be able to enhance the quality of life for patients who suffer with bowel incontinence. Sacral neuromodulation is an important tool that can help restore control, confidence and community for these individuals.”
Advertisement
Advertisement

Nonthermal technique reduces bleeding and perforation risk

Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer

PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital

Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence

Noninvasive modality gains ground in United States for patients with early-to-moderate disease

Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases

Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules

Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.