Successful transition of care for patients with pediatric cholestatic liver disease is multidisciplinary
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
With the growing number of adult patients with pediatric-onset liver disease, internists and adult hepatologists need to be aware of these liver diseases and develop expertise to manage this challenging group of patients. Moreover, young adults with pediatric-onset chronic liver disease pose distinct challenges such as pregnancy, adherence to medical regimens and psychosocial changes in life.
Young adults with pediatric liver disease are a unique cohort of patients with different evaluation and monitoring strategies, treatment, complications and comorbidities. This creates a critical need for successful transition of these patients into adult care, with incorporation of a formal transitional model and multidisciplinary team. These patients need a “transition of care” rather than a “transfer of care.” Transition of care is a multifaceted process that takes the medical, educational and psychosocial needs of the patient into consideration before switching their care to adult care physicians, whereas transfer of care is simply an administrative process of change to adult care without previous knowledge of the patients.1
Advertisement
The causes of cholestasis in children are different from those in adults. Pediatric cholestasis is caused either by genetic defects that affect the process of synthesis, processing, or secreting bile, or by mechanical obstruction of the biliary tract, the classic example being biliary atresia.
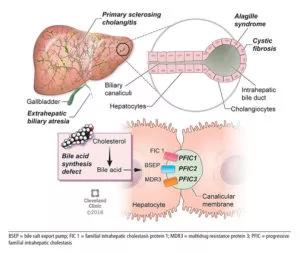
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e925f525-41d8-41f9-8f77-19abcd9ac353/805x-Inset-Selvakumar-300x253_jpg)
Cholestasis in children can be caused by biliary tract obstruction such as in biliary atresia (top) or defects in forming and excreting bile acids and other components of bile (bottom).
With the growing number of adult patients with pediatric-onset liver disease, internists and adult hepatologists need to be aware of these liver diseases and develop expertise to manage this challenging group of patients. Moreover, young adults with pediatric-onset chronic liver disease pose distinct challenges such as pregnancy, adherence to medical regimens, and psychosocial changes in life.
These patients need a “transition of care” rather than a “transfer of care.” Transition of care is a multifaceted process that takes the medical, educational, and psychosocial needs of the patient into consideration before switching their care to adult care physicians, whereas transfer of care is simply an administrative process of change to adult care without previous knowledge of the patients.2
In this article, we discuss relatively common types of inherited childhood-onset cholestatic disease and their implications and management in adulthood. Other acquired or rare cholestatic diseases are beyond the scope of this article.
Advertisement
Outcomes of liver transplant in children and adolescents have improved tremendously in the past two decades with advances in surgical techniques, pre- and postoperative management, organ preservation and immunosuppression. Now, most pediatric liver transplant recipients survive into adulthood, creating a unique challenge for internists and adult care hepatologists.2
In rebellious adolescents and young adults, risk-taking behavior, nonadherence to immunosuppressive medications, alcohol intake and substance abuse increase the risk of graft rejection and loss. Current immunosuppressive drugs such as calcineurin inhibitors (tacrolimus, cyclosporine), mycophenolate mofetil, sirolimus and corticosteroids have drastically decreased rejection rates in compliant patients.2 Educating patients on the importance of taking their medications and avoiding alcohol and drug abuse is especially important for adolescents and young adults, as rates of nonadherence are high in these age groups.
Although pregnancy is usually successful after liver transplant, it should be considered high-risk due to reported complications such as graft rejection, diabetes, preeclampsia, sepsis, prematurity and low birth weight. Conception should be avoided for at least one year after transplant.3 Appropriate counseling with regard to pregnancy and contraception is important.
Liver transplant is life-saving and improves quality of life. However, long-term pediatric liver transplant recipients face challenges such as strict adherence to medications and follow-up visits, avoiding exposure to infections and fear of graft rejection.
Advertisement
Chronic liver disease in children leads to failure to thrive, growth failure and even delayed puberty, which resolve in most patients after liver transplant before adulthood in the absence of other comorbidities.5 However, these patients are reported to have lower psychosocial functioning and more psychiatric disorders such as anxiety or posttraumatic disorder.2,5
Therefore, a psychologist or other mental health professional should be part of the management team from the time of pretransplant assessment to identify mental health problems and the need for adjustments before liver transplant. Ongoing psychosocial assessment after liver transplant is equally important to identify risks such as drug or alcohol abuse, depression, posttraumatic stress disorder and medication nonadherence, all of which can negatively affect posttransplant outcome.6
In addition, assessment of family functioning and structure is important for good long-term outcomes posttransplant; therefore, a social worker should also be a part of the transplant team. Psyschosocial assessment tools can identify high-risk candidates who would benefit from earlier intervention to avoid any negative impact posttransplant.
Neurocognitive development can be delayed in children with chronic liver disease, and the delay may persist even after liver transplant, with reported impairments in intellectual ability, language, verbal and visuospatial functioning skills.2 In spite of this, a recent study found that more than half the study patients were employed at a median follow-up of 24 years from liver transplant and a median age of 27.7
Advertisement
Remarkably, pediatric liver transplant recipients have reported quality of life comparable to that in the general population,8 and even better than in patients with other chronic illnesses.9
Key requirements for an adolescent patient include knowledge about the disease, demonstration of responsibility toward disease management and self-management of healthcare needs such as scheduling appointments or insurance needs. This demanding task could be streamlined if pediatric liver transplant programs could adopt a formal transitional model. The transition could start as early as age 10 to 12, with gradual transfer of health management responsibilities from parents to adolescents from age 13 to 17.10
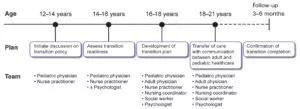
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/920fd8b7-fc98-493e-916c-e82da8fd693d/selvakumar_pediatriccholestaticliverdisease_f2-1-300x109_jpg)
A prolonged period of transition up to age 25 is preferred in complicated cases. Distinctive consideration for transition should include those with neurocognitive developmental delay from underlying disease or hepatic encephalopathy before transplant. These patients need additional support and time to achieve independence in health management before transition.11 Validated questionnaires are available to assess readiness to transition into adult care,12 implying that the decision to transition should not be based solely on age.
Please note: This is an abridged version of an article originally published in the Cleveland Clinic Journal of Medicine.
Advertisement
Findings hold lessons for future pandemics
One pediatric urologist’s quest to improve the status quo
Overcoming barriers to implementing clinical trials
Interim results of RUBY study also indicate improved physical function and quality of life
Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner
The benefits of this emerging surgical technology
Integrated care model reduces length of stay, improves outpatient pain management
A closer look at the impact on procedures and patient outcomes