A Q&A with pediatric psychologist Ethan Benore, PhD
Ethan Benore, PhD, has devoted his tenure with Cleveland Clinic Children’s to studying and applying nonpharmacological pain interventions to the treatment of children. In this article, he answers questions about how biofeedback helps his young patients (most of whom suffer from 15 or more migraine headaches per month), reducing their headache pain and frequency by half.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Q: How does biofeedback help the 10 percent of kids who experience migraines?
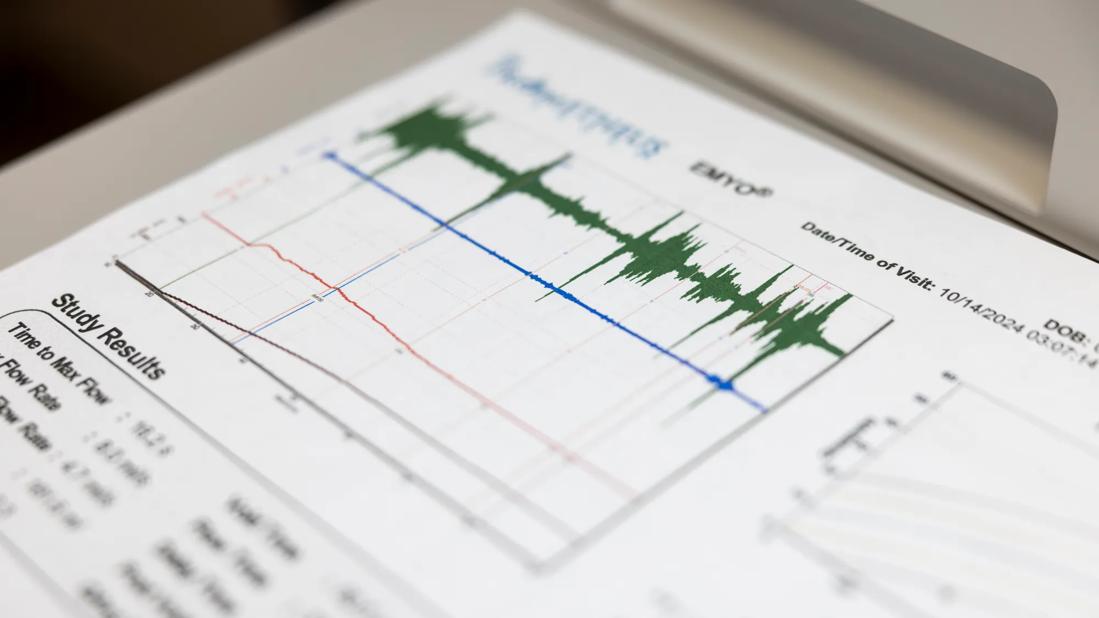
A: Biofeedback is a therapy that involves a real-time assessment of physiological processes (heart rate, blood volume, temperature, muscle activity), with signals we amplify and present to the patient as feedback. Patients interact with this information and learn to control these processes so they can impact things like headaches. For some patients, what works may be pleasant imaging; for others, paced breathing or even body posture may produce the desired effect. I tell the kids it’s like learning to wiggle your ears or flare your nostrils. You figure out which muscles make those things happen and then practice until you can do it easily.
Q: What does the biofeedback training look like for a child in your clinic?
A: In the Pediatric Pain Rehabilitation Program, we use biofeedback as a complement to behavioral therapy for most children. Learning is incremental. We start with helping them become aware of migraine triggers and changing their lifestyle habits ― things like eating, sleeping, drinking water, when and how they exercise and do their homework. Then we add the relaxation training and biofeedback component, as well as other stress management tools.
It’s a matter of experimenting with different skills, and as with everything else, practicing the things you find that work for you. In the end, the child has an action plan that represents the sum total of all the skills they have learned and how they are going to implement them to prevent headaches.
Advertisement
Q: Once the clinic sessions are over, what does the child do at home?
A: Practice! Regular practice can help the body become more resilient to migraine triggers, as well as shape new habits to avoid other triggers. Patients can use an app or even an inexpensive personal biofeedback device at home to strengthen their skills. Current research supports that just following a routine of biofeedback practice is more important than reaching any particular set point in the body.
After headaches improve, patients may continue to practice biofeedback, though they can maintain results with less frequent sessions.
Q: How old should children be before they can participate in biofeedback?
A: Most of our patients eight or older have the cognitive maturity to understand the relationship between what happens on the screen and their own body responses, so we employ this straightforward training method for most kids. For younger children, or those who struggle to make this connection, we often use biofeedback-based games to keep them engaged.
Q: How much relief can patients get from this therapy?
A: A primary goal of treatment is to reduce headache frequency and duration by 50 percent, but obviously we strive for even better outcomes. Biofeedback research and our own experience demonstrate this level of efficacy is achievable by combining biofeedback with behavioral therapy.
Q: What intrigues you about this work?
A: It’s so gratifying to help children experience relief from pain. What I love to see is that look on their face during biofeedback, that “Aha!” moment, when they suddenly realize what it feels like to coax their body into a relaxed state for the first time. I then say, “You’ve got it! Now let’s figure out how to do this all the time!”
Advertisement
Our typical patient is 14 and has an average of six migraines a week. We are campaigning to reach out to younger children with less frequent headache. If we can see these kids earlier, not only are we helping them avoid significant pain, but we are also lessening the impact these headaches have on their lives over the long run. Their healthy emotional, social, academic and family life are all at stake.
Advertisement
Advertisement

One pediatric urologist’s quest to improve the status quo

Overcoming barriers to implementing clinical trials

Interim results of RUBY study also indicate improved physical function and quality of life

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

The benefits of this emerging surgical technology

Integrated care model reduces length of stay, improves outpatient pain management

A closer look at the impact on procedures and patient outcomes

Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve