How rates of colectomy and biologics use have changed over time

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3f926ef2-daf8-4683-8fe3-d7601fa581f7/20-DDI-1983916-ACG-Decreasing-Colectomy-UC-Biologic-Medications_jpg)
20-DDI-1983916-ACG-Decreasing-Colectomy-UC-Biologic-Medications
Colectomy rates in patients with ulcerative colitis (UC) are declining as biologic therapy utilization increases, according to the largest population-based study of UC patients to date. Cleveland Clinic researchers presented the analysis of 20 years of data at the 2020 Annual Meeting of the American College of Gastroenterology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The trends revealed in this study are consistent with smaller cohort studies around colectomy rates and the advent of biologic therapies,” says George Khoudari, MD, an internist and research fellow at Cleveland Clinic’s Digestive Disease & Surgical Institute, and lead author of the abstract. “Biologics have been a game changer for the treatment of UC, and while not effective for everyone, have improved the quality of life for our patients, reducing hospitalizations and surgeries.”
Researchers mined a commercial database of 20 years of electronic medical record data from 61,592,650 patients from 26 U.S. healthcare systems. From 2000 to 2019, 146,430 patients ages 18 and older were identified as having UC according to the Systematized Nomenclature of Medicine Clinical Terms. During the entire period, 10.2% of patients had a colectomy, and 6.8% were treated with biologics, including tumor necrosis factor, integrin and interleukin inhibitors. Researchers compared the rates of colectomy and biologics use over 20 years using linear regression.
“We expected that after we controlled for other therapies, we’d see a decline in the use of colectomy over the years, but the rates of decline were more pronounced than we predicted,” says Miguel Regueiro, MD, senior author of the study and Chair of Cleveland Clinic’s Department of Gastroenterology, Hepatology and Nutrition.
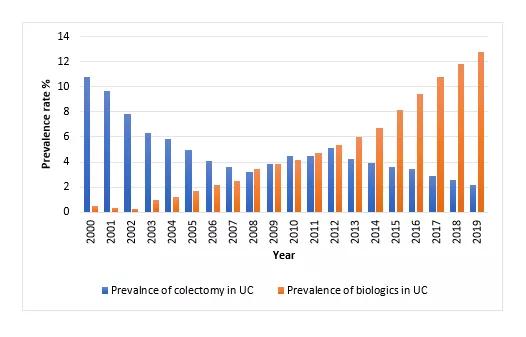
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ce81fa47-07a7-4af9-9579-7c1b9d42b043/acg-figure-khoudari_png)
The trend of colectomy and biologic use prevalence over two decades
The prevalence of colectomy declined from 10.8% to 2.1% from 2000 to 2019, respectively. At the same time, there was an associated linear increase in the prevalence of biologic usage from 0.5% to 12.8% (P < 0.001). Researchers adjusted the data to include other therapies such as mesalamine, thiopurines and corticosteroids and found that biologics were inversely related to colectomy (P < 0.001).
Advertisement
“The treatment for ulcerative colitis has changed significantly over the past 20 years with biologics being initiated earlier in the inflammatory bowel disease [IBD] course,” says Dr. Khoudari. “In this patient population, we noticed a falling trend of colectomy prevalence that coincides with a rising trend in biologics use. This is a very important observation and may change the natural course of IBD.”
This research is part of a new era of IBD care at Cleveland Clinic combining novel medical and surgical therapies with pioneering research. The outcome is IBD care that is setting a high standard, exceeding that of traditional IBD centers of excellence.
Perhaps the most fundamental shift has been the introduction of Cleveland Clinic’s IBD medical home, which pairs patients with a team of colorectal surgeons, pain specialists, pharmacists, dietitians, social workers, psychologists and others, all led by a gastroenterologist.
“While it’s still early, we’re seeing that our patients with ulcerative colitis and other inflammatory bowel diseases experience improved quality of life, decreased emergency department visits and hospitalizations, and reduced total cost of care thanks to the medical home model,” says Dr. Regueiro, who leads the program. “We plan to set the trends for treating these diseases for many years to come.”
Advertisement
Advertisement
Benefits of neoadjuvant immunotherapy reflect emerging standard of care
Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence
Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors
Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling
Potentially cost-effective addition to standard GERD management in post-transplant patients
Findings could help clinicians make more informed decisions about medication recommendations
Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care
Retrospective analysis looks at data from more than 5000 patients across 40 years