Post hoc analysis of phase 3 trial shows benefit
A subset of patients with familial adenomatous polyposis (FAP) treated with a combination of sulindac and eflornithine have a decreased risk of progression and a delayed need for lower gastrointestinal (LGI) surgery, according to a post hoc analysis of a phase 3 trial presented at the American College of Gastroenterology Annual Meeting. The post hoc analysis of results from the CPP FAP-310 trial, recently published in New England Journal of Medicine, found these benefits in FAP patients with an intact colon, ileorectal anastomosis (IRA) or ileal pouch anal anastomosis (IPAA).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
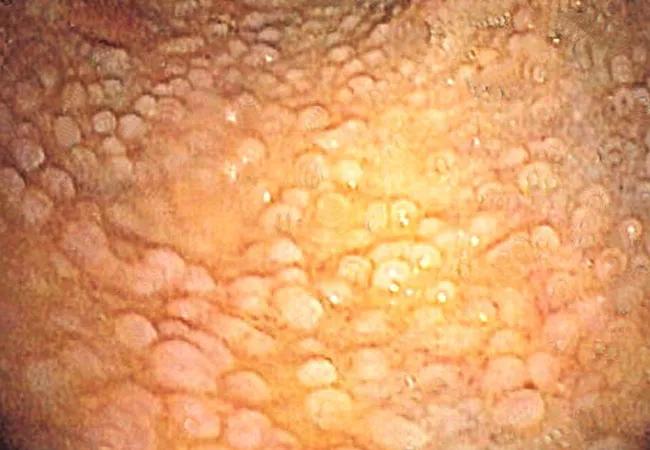
FAP is an inherited colorectal cancer (CRC) syndrome caused by a germline mutation in the adenomatous polyposis coli gene. Progression to CRC is inevitable in patients with FAP who have not undergone colectomy, with an average age of onset of 39.
“In a previous study of patients with sporadic colorectal adenomas, the combination of eflornithine and sulindac prevented over 90% of metachronous advanced adenomas. We hypothesized that a similar beneficial effect in the lower gastrointestinal tract would be seen in patients with FAP,” says James Church, MD, presenting author of the study and recently Director of the Sanford R. Weiss Center for Hereditary Colorectal Neoplasia in Cleveland Clinic’s Digestive Disease and Surgical Institute. “The results of this post-hoc analysis conformed our hypothesis.“
In the initial trial, eligible adults with FAP were randomized to eflornithine 750 mg, sulindac 150 mg or both, once daily for up to 48 months. The population for the current study was limited to the 158 intent-to-treat patients with either a native lower gastrointestinal tract or a tract reconstructed as a pelvic pouch. Patients with an end ileostomy were excluded. Efficacy analysis measured time from randomization to disease progression, which researchers defined as need for surgery, excision of polyps > 10mm and/or presence of polyps with high-grade dysplasia.
Researchers observed FAP disease progression in 3.7% of the 54 patients in the combination arm, 17% of the 53 patients in the sulindac arm, and 19.6% in the 51 patents sin the eflornithine arm. The risk reduction was thus significant for comparison of the combination therapy with both individual therapy arms, at 80% (HR = 0.20; 95% CI 0.05-0.80, P = 0.02) for combination therapy vs. sulindac and 83% (HR = 0.17; 95% CI 0.04-0.70; P = 0.01) vs. eflornithine.
Advertisement
“We were also encouraged to see reductions in the need for surgery approaching 100% in patients on the combination therapy,” says Carol Burke, MD, coauthor of the study and Vice Chair of the Department of Gastroenterology and Hepatology, Director of the Center for Colon Polyp and Cancer Prevention and Head of the Section of Polyposis in the Sanford R. Weiss, MD, Center for Hereditary Colorectal Neoplasia.
An endoscopist determined if patients met the criteria for surgical need, which was 0 in patients treated with combination therapy, 13.2% of those treated with sulindac and 15.7% of those treated with eflornithine (HR = 0.00; 95% CI 0.00-0.48; P = 0.005, and HR = 0.00; 95% CI 0.00-0.44; P = 0.003, respectively). Results were similar between precolectomy FAP patients as well as those with an IPAA or IRA.
“These promising data could add an effective option to the strategy for treatment of patients with FAP, especially for those patients with compelling reasons to defer surgery such as a high risk of desmoid disease, financial or social constraints or significant comorbidity.” says Dr. Church.
Work toward gaining FDA approval is currently in progress.
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years