Study examines open and robotic approaches for bladder cancer surgery
As robot-assisted radical cystectomy with intracorporeal urinary diversion (ICUD) has become an increasingly popular option in many high-volume centers, so too is the importance of comparing its outcomes to those of a more traditional open approach.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In a recent Cleveland Clinic led study, researchers examined the outcomes and complications of patients who underwent three surgical approaches to radical cystectomy with urinary diversion. They published their findings in The Journal of Urology.
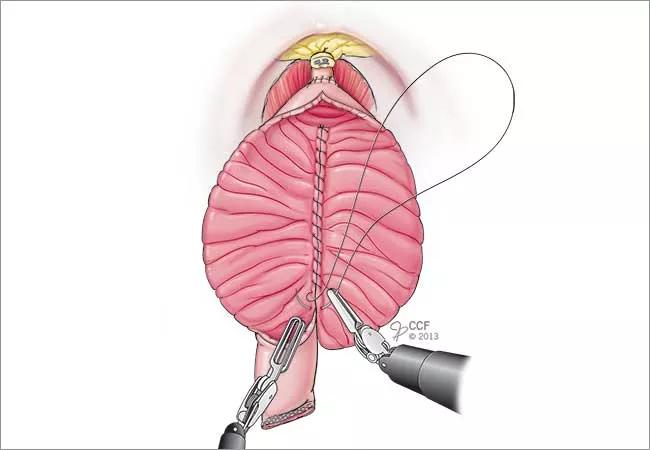
Robot-assisted cystectomy was popularized in the early 2000s and was touted as a less-invasive alternative to a traditional open cystectomy. Still, it’s not uncommon for some surgeons to take a hybrid approach, utilizing the robotic platform but reverting to an open approach for the urinary diversion part of the procedure, known as extracorporeal urinary diversion (ECUD). While more technically challenging, ICUD enables surgeons to more fully utilize the minimally invasive benefits of the robot for radical cystectomy.
“While ICUD is certainly an innovative approach utilized by bladder cancer surgeons, we recognize it’s not the only approach,” says Byron Lee, MD, PhD, a urologist in Cleveland Clinic’s Glickman Urological & Kidney Institute and senior author of the study. “In the context of patient outcomes, a direct comparison of these approaches is not well-described in the literature. That is what we hoped to contribute with this study.”
The study examined the perioperative and pathological outcomes of 948 patients who underwent radical cystectomy with urinary diversion and bilateral pelvic lymph node dissection at Cleveland Clinic from 2011 to 2018.
This included 272 cases of open radical cystectomy (ORC), 301 with ICUD, and 375 with ECUD. Perioperative and pathologic outcomes were evaluated, as well as complications at 30- and 90-day intervals.
Advertisement
Notably, the authors found that estimated blood loss was lower for the ICUD method (p <0.001). Further, ICUD cases demonstrated shorter hospitalization (p <0.001) and a lower rate of postoperative ileus (p = 0.023), a common gastrointestinal complication associated with radical cystectomy.
In fact, overall, the study showed that the ICUD approach was associated with lower complication rates at 30- and 90-days, respectively, than the alternative procedures. However, readmission rates remained statistically similar among all three approaches.
To bladder cancer surgeons who favor the ICUD technique, these findings likely come as no surprise. “This research underscores what we have understood anecdotally for years,” says Dr. Lee. “Yes, the ICUD technique can be technically challenging, but there are significant clinical benefits for patients.”
When it comes to controlling cancer, research has shown that there is no significant difference between traditional open and robot-assisted modalities. With that in mind, Dr. Lee stresses that the best approach is often context-dependent and may simply depend on independent patient factors and the surgeon’s training and preference.
Although, studies like this that demonstrate comparative outcomes will likely support the continued use of ICUD within the field. Dr. Lee concludes, “It is a well-utilized technique at Cleveland Clinic, where we handle among the highest volumes of robot-assisted cystectomies using ICUD. We are committed to continue exploring minimally invasive techniques to improve patient outcomes and also to training the next generation of bladder cancer surgeons on this platform.”
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient