New program is tracking lung nodules across the enterprise
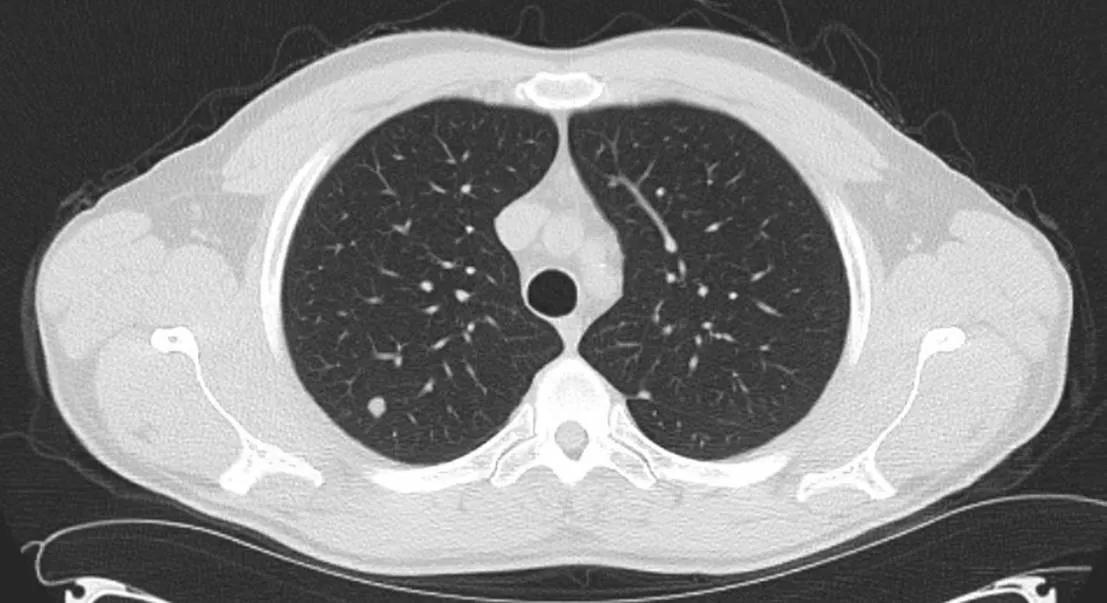
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c5fd534b-b119-4283-80b3-e22df1e6342c/21-PUL-2048527_jpg)
21-PUL-2048527
By Peter Mazzone, MD, MPH; and Louis Lam, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Lung nodules are one of the most common incidental findings seen on radiology exams. Concerns arise when these nodules go unrecognized as may occur if the imaging study is not performed for a pulmonary complaint or if the ordering provider is not involved in the longitudinal care of the patient. By the time the nodule is recognized, early-stage lung cancer may have become more advanced and more difficult to cure.
Separately, lung nodule management is quite nuanced. Even if an incidental lung nodule is recognized, the provider in charge of the patient’s care may not be comfortable with the next management step. In addition, the radiologist’s recommendation for guideline-based management of the nodule may be made without knowledge of the existence of prior imaging or of a patient’s medical history – both of which can significantly influence management. The result could be over-testing of benign lung nodules and delayed identification of early-stage lung cancer.
For these reasons, we have worked to develop a lung nodule management program capable of tracking all actionable lung nodules throughout our health system, while ensuring care path compliant management in accordance with the most updated guidelines.
The lung nodule management program is a partnership of individuals from multiple institutes and with a variety of skill sets all working towards the same goal:
Advertisement
To date, our pilot program with the HVTI has identified approximately 100 patients per month with incidental nodules deemed actionable by our radiologists. The flowchart shows branch points in patient management from the time they are identified to an endpoint in their care (Figure). Approximately 3% to 4% of those seen by program providers have been diagnosed with a lung cancer.
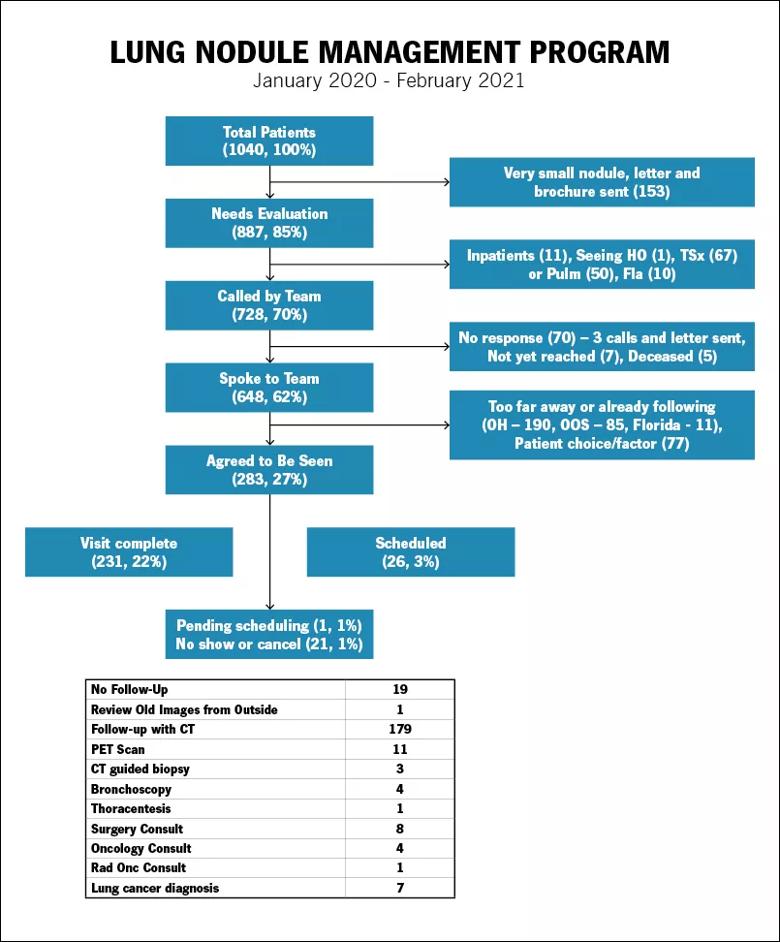
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2bb0b377-f941-47c5-abd7-efb6002c891d/805x-Inset-Lung-Nodule-Management-Program-1_jpg)
Figure. The flowchart shows branch points in patient management from the time they are identified to an endpoint in their care. Approximately 3% to 4% of those seen by program providers have been diagnosed with a lung cancer.
We are in the process of expanding this pilot program to include all patients with actionable nodules across our health system in Northeast Ohio, and we are assisting our Florida sites with the development of their own program. Over 200 patients each week are identified as having an incidental lung nodule at the enterprise level. We are applying lessons from our HVTI pilot project and using the partnerships developed with the above-mentioned provider groups to ensure we can scale up the program to the benefit of our patients and providers.
Challenges remain, including the potential for holes in the safety nets. For example, a nodule has to be identified to be flagged; a nodule has to be flagged to enter into the program; very small nodules may not be labeled actionable. There is also a need to resource the program with adequate personnel and the refinement of our population management system so that it remains functional at scale.
Advertisement
The early successes of this program and the support we have received from leaders across institutes have energized the team to take on these challenges. Ultimately, this program may serve as a model for programs addressing other actionable findings (e.g. pancreatic lesions, thyroid nodules, etc.) across our health system resulting in improved care of our patients. Expanding these programs beyond our system to assist patients and providers in resource-limited locations through the use of telehealth is a future goal.
About the authors: Dr. Mazzone is Director of the Lung Cancer Program and Lung Cancer Screening Program for the Respiratory Institute; Dr. Lam is a pulmonologist and critical care physician in the Respiratory Institute.
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program