Combination imaging, genetic testing prove invaluable
By Audrey Rhee, MD; Nima Almassi, MD; and Steven Campbell, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
It was a classic case of an incidental finding on computed tomography. A scan for appendicitis revealed two renal neoplasms in a 12-year-old previously healthy girl.
After her laparoscopic appendectomy, her physicians performed a renal mass biopsy (RMB). Pathology demonstrated an oncocytic renal epithelial neoplasm, a generally indolent tumor, and she was referred to Cleveland Clinic Glickman Urological & Kidney Institute’s pediatric urology section.
While her medical history was otherwise unremarkable, there was a history of renal malignancy in her family — in her maternal great-grandfather — and a history of neurofibromatosis type I on her mother’s side. Her paternal grandmother had renal cysts and pneumothorax.
The patient’s physical exam was normal and urinalysis was negative for hematuria or infection. Her abdominal CT demonstrated multiple simple renal cysts and two solid enhancing right lower pole renal neoplasms measuring 2.0 and 1.8 cm in greatest dimension (Figures 1A, 2A).
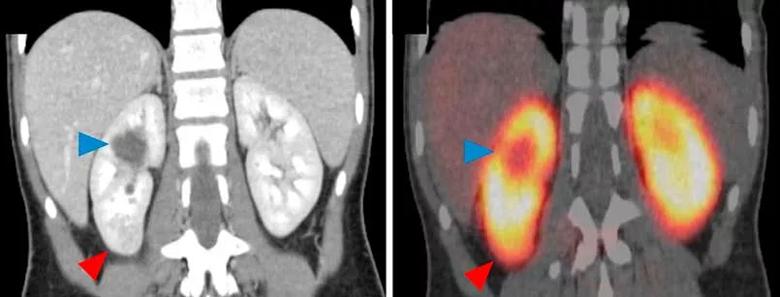
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8085ebaa-900e-4342-b96c-462fa9780c7c/805x-Inset-1_jpg)
Figure 1. (A) Coronal contrast-enhanced computed tomography demonstrating a 2.8-cm, solid enhancing renal mass in the lower pole of the right kidney (red arrowhead). The patient also has a renal cyst in the upper pole (blue arrowhead). (B) On 99mTc-sestamibi single-photon emission computed tomography/x-ray computed tomography, the lower pole lesion accumulated radiotracer at a level similar to that of the renal parynchyma (red arrowhead). This pattern of uptake is consistent with a benign renal oncocytoma or a hybrid oncocytic/chromophobe tumor. The upper pole cyst does not accumulate radiotracer and appears as a photopenic defect (blue arrowhead).
Advertisement
We referred her for counseling in our Center for Personalized Genetic Healthcare and testing with the GeneDX renal panel (GeneDx, Gaithersburg, MD).
Genetic testing revealed a fumarate hydratase deficiency. This, along with certain pathogenic variants in the fumarate hydratase gene, can be associated with hereditary leiomyomatosis and renal cell carcinoma (HLRCC) syndrome and aggressive malignancy.1
HLRCC features include:
At this juncture, we faced a clinical dilemma. RMB results suggested a relatively indolent or benign renal neoplasm, while genetic testing suggested something with far greater malignant potential. We were also aware that RMB is not as accurate as we would like in distinguishing between low- and high-grade tumors.
Faced with these diagnostic limitations, we turned to our Department of Diagnostic Radiology colleagues for assistance. Together we decided upon a 99mTc-sestamibi SPECT/CT scan, in hopes that we would obtain additional information to help us counsel this family.
The radiotracer used in this SPECT/CT combination scan accumulates in mitochondria. Mitochondria are abundant in oncocytoma and hybrid oncocytic/chromophobe tumors (HOCTs). As a result, this type of scan has been shown to have high specificity and sensitivity in discriminating benign oncocytomas and HOCTs from other renal neoplasms.2
Advertisement
The scan demonstrated radiotracer accumulation in both solid neoplasms similar to the adjacent normal parenchyma, consistent with HOCTs (Figures 1B, 2B).
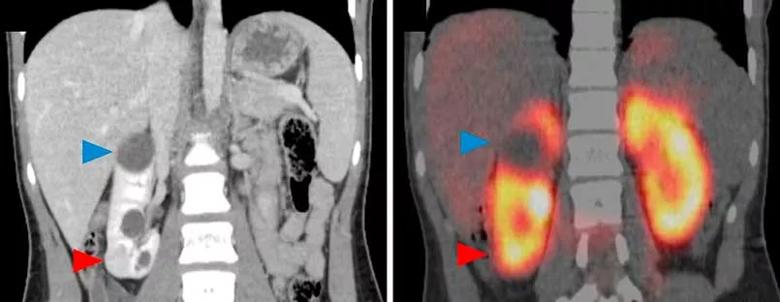
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f81dc97d-f92f-46fb-a10d-eb90cafbc04a/805x-Inset-2_jpg)
Figure 2. (A) Coronal contrast-enhanced computed tomography demonstrating a second, smaller 2.0-cm, solid enhancing renal mass in the lower pole of the right kidney (red arrowhead), as well as an upper pole renal cyst (blue arrowhead). (B) On 99mTc-sestamibi single-photon emission computed tomography/x-ray computed tomography, the lower pole mass accumulated radiotracer in a fashion consistent with a benign renal oncocytoma or a hybrid oncocytic/chromophobe tumor (red arrowhead). In contrast, the upper pole cyst appears as a photopenic defect (blue arrowhead).
Though both tumors appeared to be benign or indolent neoplasms, the family chose robotic partial nephrectomy, considering family history and genetic predisposition. To maximize nephron preservation in this young patient, we felt comfortable planning an enucleative resection.
Warm ischemia time was 23 minutes. Blood loss was 150 mL and our patient’s postoperative course was uneventful. She was discharged home on postoperative day two.
Final pathology demonstrated two HOCTs measuring 2.8 and 2.0 cm in largest dimension, with negative surgical margins. Our patient required no further treatment, but will require lifelong serial MRIs.
Pediatric renal cell carcinoma (RCC) is a rare malignancy with genetic underpinnings and biologic behavior that differ from adult RCC. It is typically diagnosed in the second decade of life.
Advertisement
Traditional imaging modalities do not adequately distinguish RCC from benign or indolent renal neoplasms, such as oncocytoma or HOCT.
This case study demonstrates the value of 99mTc-sestamibi SPECT/CT scanning in differentiating malignant and indolent from benign tumors in a pediatric patient presenting with enhancing renal neoplasms.
The case, published in the March 2018 issue of Urology, also demonstrates the value of genetic testing and counseling as an important aspect of a child’s diagnostic workup. As in this case, up to 30 percent of children with renal tumors exhibit manifestations of familial RCC syndromes.3
Dr. Almassi is former Chief Urology Resident at Glickman Urological & Kidney Institute.
Figures reprinted from Urology, Vol. 113; Almassi N, Kaouk J, Campbell SC, Rhee A, et al; Use of 99mTc-sestamibi single-photon emission computed tomography/x-ray computed tomography in the diagnosis of hybrid oncocytic/chromophobe tumor in a pediatric patient; pp. 206-208, 2018, with permission from Elsevier.
References
Advertisement
Advertisement

Findings hold lessons for future pandemics

One pediatric urologist’s quest to improve the status quo

Overcoming barriers to implementing clinical trials

Interim results of RUBY study also indicate improved physical function and quality of life

Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner

The benefits of this emerging surgical technology

Integrated care model reduces length of stay, improves outpatient pain management

A closer look at the impact on procedures and patient outcomes