Disease-modifying medications, haploidentical transplant and gene therapies
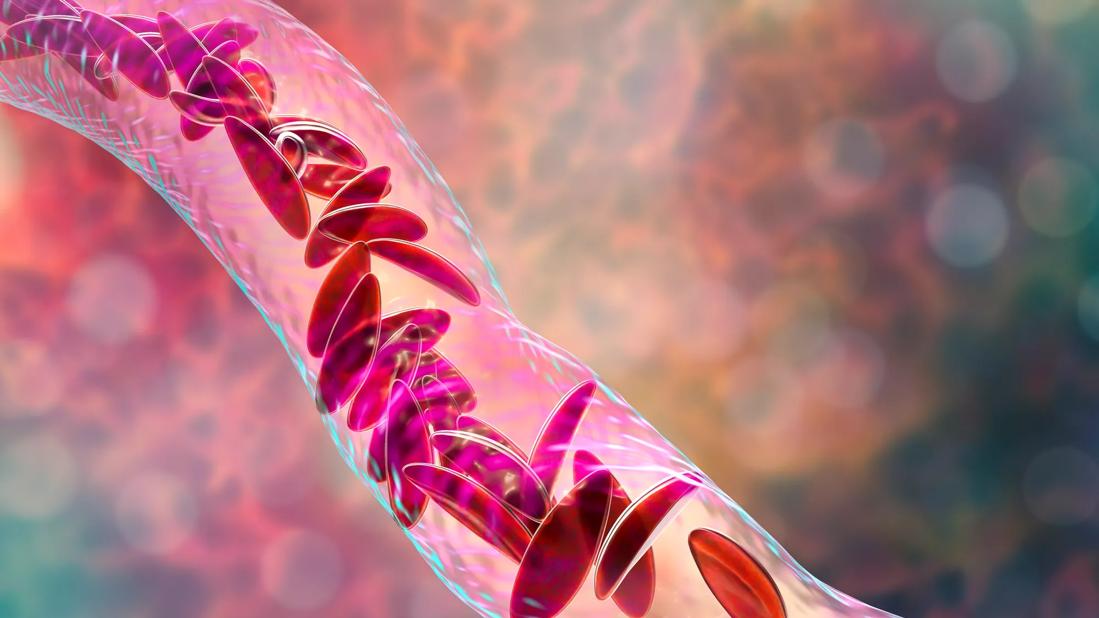
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5672314f-8ce6-4f9d-afe4-5edc45b8dce7/GettyImages-1059145434-jpg)
SCD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
It’s a very exciting time for those who treat sickle cell disease. After nearly 20 years with one option for managing disease symptoms in our patients, the last several years have brought some significant advancements.
Our understanding of sickle cell disease has improved. We now know it not only affects red blood cells, but it is the interaction with the vessels makes it a vascular disease that can affect many organs, including the lungs, heart, kidneys and liver. In addition, we have several new treatment options to offer our patients to (a) control the disease; and (b) cure the disease.
In November 2019, the FDA approved two disease-modifying medications that may decrease hospitalizations and improve quality of life for patients with sickle cell disease. Prior to these approvals, hydroxyurea was our only option.
Voxelotor is once-daily, oral inhibitor of sickle hemoglobin (HbS) polymerization. In the phase 3 clinical trial, patients taking voxelotor had increased hemoglobin levels and reduced markers of hemolysis. While it will be important to look at the long-term effects of the medication, this is a great initial response.
Another medical treatment for sickle cell disease approved in late 2019 — crizanlizumab — addresses one of the most common problems in patients with sickle cell disease: the pain crisis. Crizanlizumab, a humanized, anti-P-selectin monoclonal antibody, is a monthly injection that helps to prevent vaso-occlusive crises. In the phase 2 clinical trial, researchers found that nearly 45% of patients who received this medication had fewer pain crises and 40% fewer days in the hospital compared with the placebo group.
Advertisement
Allogeneic hematopoietic stem cell transplantation for sickle cell patients was first reported in 1984. Unfortunately, its use is limited by a dearth of HLA matched donors, the risk of developing graft-versus-host disease and long-term toxicities. There is some excitement about the ability to expand the donor pool using a transplant from the patient’s mother, father or sibling with only a half-match. At Cleveland Clinic Children’s, we are part of a multi-center clinical trial to study the feasibility of achieving a high rate of event-free survival in patients with sickle cell disease and HLA-haploidentical donors. The multi-center clinical trial is enrolling rapidly, and we hope to publish outcomes in the next year or two. Preliminary data from other transplant studies in Europe and the United States indicate that this regimen is very well tolerated and successful in curing sickle cell disease long term.
Additionally, the last several years have brought the possibility of curative gene therapy for sickle cell disease. In gene therapy, bone marrow cells are removed from the patient, genetically modified and then reinserted after the patient receives a conditioning chemotherapy regimen. The benefit of the gene therapy is that it uses the patient’s own cells; thus, the risk of graft-versus-host disease does not exist, but there is still concern and risk for possible rejection and persistence of the genetically modified cells. It is similar to technology used to treat beta-thalassemia, which received a breakthrough designation from the European Medicine Agency.
Advertisement
The costs and long-term efficacy of gene therapy for sickle cell disease remain unknown. But we are excited. There is reason to hope that we will continue to see dramatic changes in the treatment of sickle cell disease this decade — perhaps in the next five years — that will enable us to offer a cure to more patients.
Dr. Hanna is Chair of the Department of Pediatric Hematology, Oncology and Blood and Marrow Transplantation at Cleveland Clinic Children’s.
Advertisement
Advertisement
Findings hold lessons for future pandemics
One pediatric urologist’s quest to improve the status quo
Overcoming barriers to implementing clinical trials
Interim results of RUBY study also indicate improved physical function and quality of life
Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner
The benefits of this emerging surgical technology
Integrated care model reduces length of stay, improves outpatient pain management
A closer look at the impact on procedures and patient outcomes