Quality improvement efforts yield measurable results

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/581b3702-dac7-4de5-a2e5-f9b87d07898f/650x450-Intubation_jpg)
650×450-Intubation
Integrating quality improvement and safety into the culture of the pediatric critical care unit at Cleveland Clinic Children’s has contributed to standardized mortality rates that are significantly below peers, according to Samir Latifi, MD, Chair of the Department of Pediatric Critical Care Medicine.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“We standardized our approaches to many aspects of critical care, including central line infection rates, sedation protocols and extubation readiness assessment. We’ve really taken many different elements of what we call quality in critical care, and changed our culture,” Dr. Latifi says. “Our outcomes speak for themselves: our standardized mortality rates are below those of our peers, and in 2018, we had no instances of mortality in post-operative cardiac surgery patients.”
Cleveland Clinic Children’s is part of Virtual Pediatric Systems, LLC (VPS), a national organization with over 135 hospital members that collects pediatric critical care data for quality improvement purposes. Among other datapoints, VPS has developed a standardized mortality ratio using the Pediatric Index of Morality (PIM3) North America risk of mortality compared with observed mortality. In order to identify opportunities for quality improvement, VPS compares the unit in question to a reference group composed of similar patient populations (both in terms of size and mix of patients).
Hospitals aim to keep their standardized mortality rates at or below 1.0, which means that observed mortality and expected mortality are equal. For the time period from October 1, 2018 through June 30, 2019, the standardized mortality ratio was 0.58 for Cleveland Clinic Children’s, which was significantly below the peer group.
“I think our efforts to create a culture of openness while driving quality is a significant component of this improvement,” Dr. Latifi notes.
Advertisement
One project that illustrates the quality improvement projects at Cleveland Clinic Children’s addresses unplanned extubations. Unplanned extubations can lead to complications, including aspiration, respiratory distress, laryngeal edema and death. As a result, many ICUs consider unplanned extubation as a marker of quality.
“When a patient is on a ventilator and the breathing tube comes out, it can lead to a period of instability and high risk,” Dr. Latifi says. “In an ideal world, patients are awake, alert, following commands and weaned from sedatives before extubation. Achieving this requires striking a balance with sedation levels. Too much sedation, and you may sit around all day waiting for a patient to wake for extubation. If there is too little sedation, a patient may regain consciousness, become agitated and self-extubate.
“As we contemplated quality improvement projects in late 2017, we thought that our unplanned extubations were on the high side, so we formed a working group that included an attending physician and a fellow, as well as representatives from nursing and respiratory therapy,” Dr. Latifi explains.
The group reviewed the situations that led to unplanned extubations and formulated an improvement plan. A variety of factors can contribute to unplanned extubation, including staffing levels, inadequate sedation and variation in breathing trials.
“We changed our approach,” says Dr. Latifi. “Now, when a patient needs a chest x-ray, we ensure that both a nurse and a respiratory therapist (RT) are present so that the breathing tube isn’t dislodged as the patient is moved. The RT focuses on the breathing tube while the nurse moves the patient; there’s a coordinated effort to ensure that nothing untoward happens.”
Advertisement
“We also found that sedation guidelines can be vague, and we wanted to minimize that variation in our practice. We needed a unified, standardized approach to assess the level of sedation. Our working group reviewed the literature to identify a more robust scoring system, and then instituted the State Behavioral Scale. There was a lot of education of our Staff and caregivers to let them know that we were committed to the sedation protocol, that we were going to stick to a few basic drugs and get to know how to use them really well.”
“At the same time, we gathered our RTs, the Quality Officer and the Medical Director for Respiratory Therapy to discuss how they decide when a patient is ready for weaning and extubation,” Dr. Latifi continues. “The team developed a worksheet to be used daily when evaluating a patient’s progress. Has the patient reached the specific endpoints? Are they ready for a breathing trial? If you assess patients every day in a consistent manner, you can ensure that patients aren’t oversedated and minimize time on the ventilator.”
Breathing trials are another hot topic in both adult and pediatric intensive care units (ICUs). “If I meet 10 ICU doctors, they might have 10 different ideas about what counts as a breathing trial. We needed to get to the point at which we know exactly what’s been done when someone says they’ve done a breathing trial. And each physician has to adapt their practice so that there’s uniformity in care,” Dr. Latifi states.
By assessing and documenting progress regularly, Dr. Latifi’s group found that extubation was more controlled. “By implementing these tactics, we saw change pretty quickly. We brought the number of unplanned extubations per 1,000 vent days down from 18 in 2016 to 4 in 2019,” Dr. Latifi says.
Advertisement
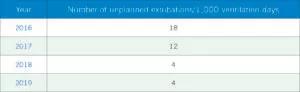
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c5013c49-ddf3-4412-9437-0a35cbe3b7e2/Extubations-300x92_jpg)
Dr. Latifi’s experience with improvement projects illustrates how standardizing an approach drives quality. “It really gives our caregivers an opportunity to speak up and say, ‘Hey, this doesn’t follow the guideline,’” Dr. Latifi concludes.
Advertisement
Advertisement
Findings hold lessons for future pandemics
One pediatric urologist’s quest to improve the status quo
Overcoming barriers to implementing clinical trials
Interim results of RUBY study also indicate improved physical function and quality of life
Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner
The benefits of this emerging surgical technology
Integrated care model reduces length of stay, improves outpatient pain management
A closer look at the impact on procedures and patient outcomes