With 5-year results now in, a lead investigator looks ahead
Five-year results of the ABSORB III clinical trial suggest that the excess risk associated with bioresorbable vascular scaffolds (BVS) compared with everolimus-eluting stents (EES) ends at three years. For many in the field, these findings offer some hope for the technology’s future.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Stephen Ellis, MD, Director of Interventional Cardiology at Cleveland Clinic and lead investigator of ABSORB III, is among the cautiously optimistic. He presented the data at TCT 2019 and is coauthor of the recent report of the five-year results in Circulation. Consult QD spoke with Dr. Ellis about whether the latest results will spark renewed interest in the technology and what’s ahead for BVS.
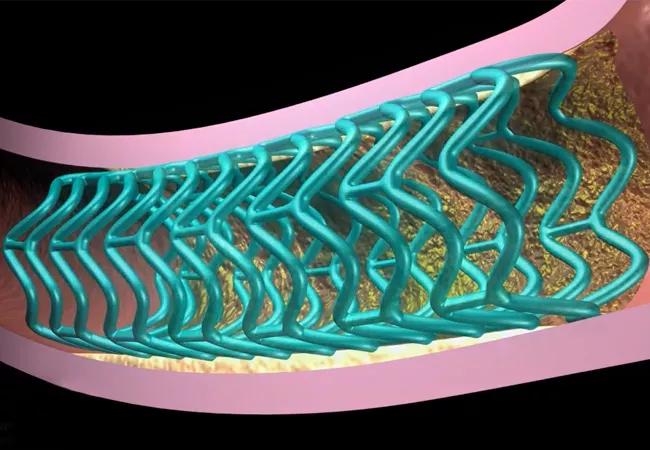
Dr. Ellis: The original value proposition of bioresorbable scaffolds was to provide a comparable clinical result to drug-eluting stents up until the time the scaffold dissolved. After it dissolved, you would have a vessel unencumbered by residual metal stent, avoid adverse stent-related events and get better results overall. But our three-year results showed unacceptable levels of target lesion failure, death, revascularization and myocardial infarction. The device was pulled from the market, and many wrote off the technology for good.
But when we published those results, the scaffolds had not yet dissolved. The five-year results confirm that the elevated risk neutralizes after scaffold resorption. The results are underpowered due to the small number of events that occurred between years 3 and 5, so we can’t say for certain, but we do see the basic concept playing out. Those of us who had not yet given up on the original value proposition are hoping these results push the field forward in developing a better scaffold.
Dr. Ellis: Right now, several are in development. Hindsight shows us that the struts on the original scaffold were too thick at 150 microns. Strut thickness of current drug-eluting stents is between 60 and 80 microns. Products with struts of about 100 microns are in development, and the idea is that these are less inherently thrombogenic than the larger struts. Polymers that biodegrade faster and magnesium-based devices are also under investigation. But the scaffold itself is only part of the issue; patient selection and operator technique are also important.
Advertisement
Dr. Ellis: A key take-home from our two-year results was that BVS shouldn’t be used in very small vessels. The results showed that the BVS is generally comparable to the EES when the device is placed in appropriately sized vessels using appropriate procedural techniques. So vessel choice is key.
Another area we’re exploring is whether advanced imaging is necessary to ensure the device is sized correctly for the vessel. The use of optical coherence tomography, or OCT, allows more precise measurements than the original study protocol, which allowed physicians to determine vessel size based on visual assessment from coronary angiography.
Procedurally, post-dilatation produces better outcomes, but it wasn’t mandated in ABSORB III. In ABSORB IV, we strongly suggest in the protocol that post-dilatation should be performed at high pressure — at least 16 to 18 atmospheres — and the balloon-to-scaffold ratio ought to be at least 1.1 to 1 unless the scaffold appears to be oversized after initial implantation. We’re following the moniker PSP — P for predilatation (which we’ve always championed), S for appropriate sizing and the second P for adequate pressure with post-dilatation.
Dr. Ellis: Five-year results of ABSORB III offered a few key insights, but ultimately we’ll need more patients and longer follow-up to make an assessment of the original value proposition of BVS. The question of whether the bioresorbable device confers a benefit likely won’t be definitively answered until seven years after ABSORB IV recruitment ends — which means early 2025. I am also interested to see the seven-year follow-up data for COMPARE-ABSORB, which was stopped early based on results from ABSORB II and III.
Advertisement
For many of my colleagues, the bioresorbable scaffold story ended with the three-year results of ABSORB III. While those results certainly put a damper on things, I think five-year results demonstrate that we shouldn’t shut the book just yet.
Dr. Ellis’ colleague Samir Kapadia, MD, concurs. “BVS came to market with great promise and very high expectations, and then left very quickly, creating disappointment,” says Dr. Kapadia, Chair of Cardiovascular Medicine at Cleveland Clinic. “However, the truth is somewhere in between, with continued evolution of BVS technology likely to have an important niche role in percutaneous interventions.”
ABSORB III is funded by Abbott Laboratories.
Advertisement
Advertisement

How Cleveland Clinic is using and testing TMVR systems and approaches

NIH-funded comparative trial will complete enrollment soon

How Cleveland Clinic is helping shape the evolution of M-TEER for secondary and primary MR

Optimal management requires an experienced center

Safety and efficacy are comparable to open repair across 2,600+ cases at Cleveland Clinic

Why and how Cleveland Clinic achieves repair in 99% of patients

Multimodal evaluations reveal more anatomic details to inform treatment

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more