Taking steps toward standardizing prevention and management
By Marie Budev, DO, MPH, and Michael Machuzak, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Early in the history of lung transplantation, airway complications were recognized as a major contributor to morbidity and mortality. Improvements in lung preservation, surgical techniques and perioperative management have led to a decrease in the incidence of airway complications, but they continue to adversely impact outcomes following transplantation. The incidence of airway complications has been reported to be in the range of 2 to 18 percent, with this marked variability attributed to lack of standardized definitions for diagnosis.
Airway complications, in the form of dehiscence, stenosis or malacia, most commonly involve the bronchial anastomosis, but the latter two complications also can involve the bronchial tree distal to the anastomosis. While initially encountered in the early post-transplant period, airway complications can persist as a chronic, recurrent problem throughout the post-transplant course.
Recently, we were invited by the International Society for Heart and Lung Transplantation to join the Airway Complications Workgroup, comprised of experts in lung transplantation and interventional pulmonology from around the world. The Airway Complications Workgroup developed and published the first consensus statement on airway complications after lung transplantation. This consensus statement provides clear definitions of the common airway complications and also proposes a new adult and pediatric grading system based on the location and extent of ischemic injury, dehiscence and stenosis.
Advertisement
In addition to standardizing definitions and grading of complications, the intent of the consensus statement is to facilitate dialogue between pulmonologists and interventional bronchoscopy teams in developing standardized approaches to prevention and management of these complications.
With extensive experience in both lung transplantation and interventional pulmonology, Cleveland Clinic physicians and surgeons have been at the forefront of developing strategies to address airway complications. Our surgeons pioneered and investigated the impact of bronchial artery revascularization in reducing the risk of airway complications. Our interventional pulmonologists perform more than 250 procedures annually for airway complications after transplantation and also benefit from extensive experience in treating other benign and malignant airway disorders. This experience has allowed our team to introduce novel approaches, including use of uncovered metallic stents and amniotic membrane grafts in treating bronchial dehiscence after transplantation. Additionally, technical innovations, such as in vivo modification of stents and custom 3-D printed stents, developed by our team for airway complications in other patient populations now can be applied to management of post-transplant airway complications.
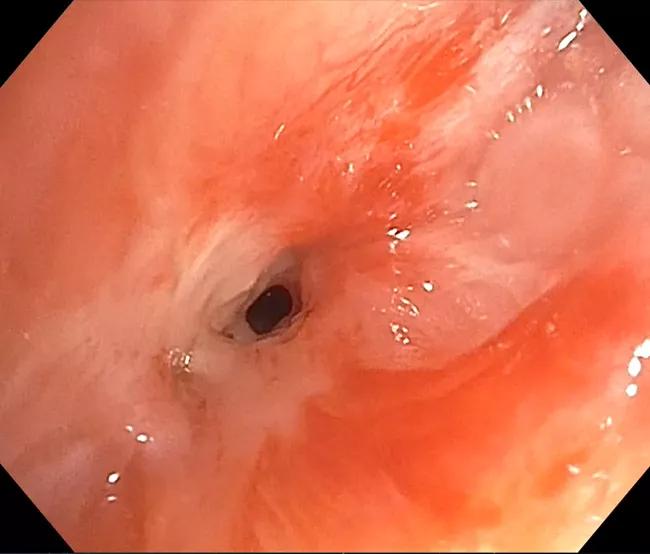
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5921d027-d17f-45b6-9e94-4a2b6dd8f30c/18-PUL-4731-Budev-Inset-01-650pxl-width_jpg)
A patient suffered from severe refractory bronchial stenosis S/P B/L lung transplant. Stenosis involved RBI, RML and RLL superior segment. Multiple attempts were made to preserve segments.
Advertisement
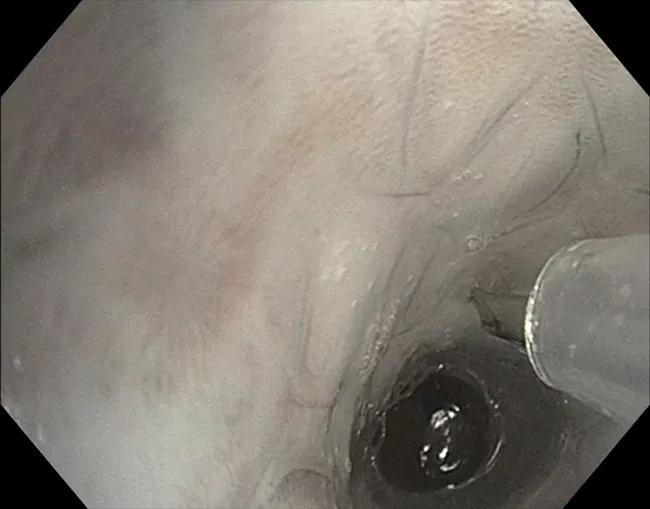
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/61c0aefc-c651-4c1a-bc84-127dd64de291/18-PUL-4731-Budev-Inset-02-650pxl-width_jpg)
Primary stent is placed and needle is used to poke hole in location or RML.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e8c131a5-7534-4da6-a525-f03bd8b9341b/18-PUL-4731-Budev-Inset-03-650pxl-width_jpg)
Balloon dilation of newly created “airway” to RML
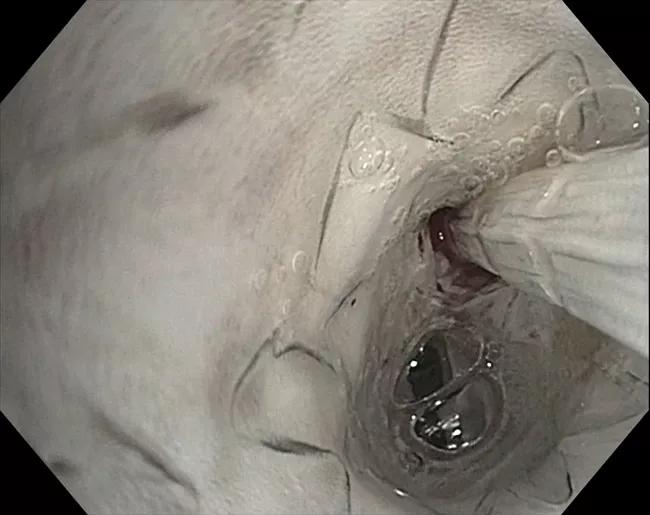
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6d1b97b1-1641-4b7b-9621-350b441f69c6/18-PUL-4731-Budev-Inset-04-650pxl-width_jpg)
Stent in stent placement.
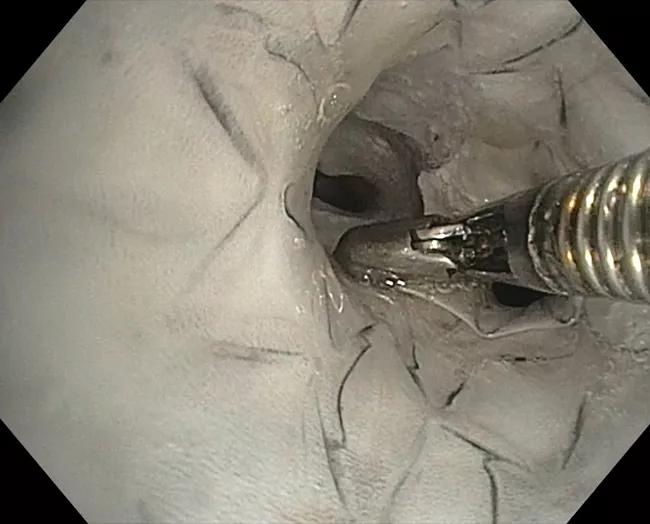
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/75b3b887-6f6e-40f9-b93a-82761a79d6ad/18-PUL-4731-Budev-Inset-05-650pxl-width_jpg)
Minor adjustments made to stent allowing for ideal fit.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/91036ea4-f263-4c43-aea4-f60e142ff9d0/18-PUL-4731-Budev-Inseet-06-650pxl-width_jpg)
Final result. In vivo stenting allowed for two additional years of airway patency with reduced procedures until patient unfortunately died in a motor vehicle accident almost eight years after transplant.
The combination of a successful, high-volume lung transplant program and an experienced interventional pulmonology team has positioned Cleveland Clinic to be a leader in the management of post-transplant airway complications. Through experience and innovation, we hope not only to develop effective treatment strategies but also techniques to mitigate the risk of developing these complications.
Dr. Budev is the Medical Director of Lung Transplantation and holds the Macon and Joan Brock Endowed Chair for Lung Transplantation.
Dr. Machuzak is staff in the Department of Pulmonary Medicine.
Advertisement
Advertisement

Recent breakthroughs have brought attention to a previously overlooked condition

A review of treatment options for patients who may not qualify for surgery

Looking at the real-world impact and the future pipeline of targeted therapies

The progressive training program aims to help clinicians improve patient care

New breakthroughs are shaping the future of COPD management and offering hope for challenging cases

Exploring the impact of chronic cough from daily life to innovative medical solutions

How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program

Collaborative patient care, advanced imaging techniques support safer immunotherapy management