New research aims to improve suboptimal lung transplant outcomes by “looking beyond the walls of hospitals”

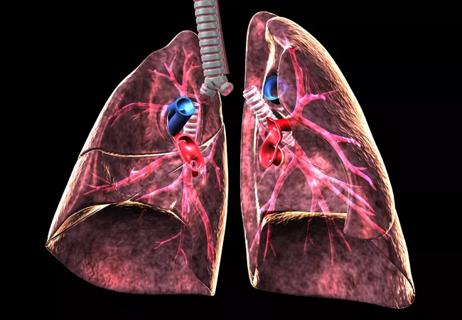
Lung transplant is a lifesaving surgery for patients with fatal lung diseases such as chronic obstructive pulmonary disease (COPD), pulmonary fibrosis or pulmonary hypertension. However, a critical limitation exists as the national median post-transplant survival is merely 5.5 years which is sometimes only half the survival experienced by other organ transplant types. This suboptimal survival is from the accelerated deterioration in lung function in the years after transplant, otherwise known as chronic rejection, and this cannot be entirely explained by transplant center practices, donor factors or recipient factors alone.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
To address this gap, researchers at Cleveland Clinic were awarded an R01 $3.2 million grant from the National Heart, Lung, and Blood Institute (NHLBI) for their project, “A place-based approach to geographic differences in lung transplant.” The grant is multiyear, and the researchers will leverage a geospatial sciences framework to measure, map and model the effects neighborhoods have on lung transplant.
“Chronic rejection remains the Achilles heel limiting successful long-term lung transplant survival,” according to Wayne Tsuang, MD, PhD, principal investigator of the research project, and staff physician in the Department of Pulmonary & Critical Care within the Integrated Hospital Care Institute at Cleveland Clinic.
The investigators hypothesize that neighborhood-based factors, defined as an environmental and social location with meaning to a person, impact the suboptimal survival of lung transplant recipients. However, before applying the geospatial sciences to lung transplant, a key methodologic approach must also be addressed.
Researchers have long known that a person’s place of residence has an important role on health outcomes. The most frequently used spatial unit to measure patient neighborhoods has been the postal zip code; however, zip codes come with several limitations. A zip code population averages 10,000 people and the boundaries are regularly changed by the U.S. Postal Service to facilitate delivery of mail and packages. The large size and fluid boundaries of zip codes limit a researcher’s ability to accurately measure the effect of a neighborhood on health outcomes. Unfortunately, large national transplant registries that collect a wealth of clinical information only collect zip codes, which limits progress in our understanding of health and neighborhood.
Advertisement
“Fortunately, there are more detailed spatial units called census tracts; each has an average population of 4,000 people with boundaries that are adjusted only after the decennial U.S. census,” says Dr. Tsuang. “Census tracts offer a more rigorous approach to measuring the relationship between neighborhood and health outcomes but have received little attention within clinical pulmonary research.”
One goal of this research is to create a novel multicenter geocoded registry at the census tract level from which scientists can better assess what patients are exposed to and more precisely risk stratify patients to develop targeted interventions. “Ultimately, the long-term goal is to improve the suboptimal lung transplant outcomes by looking beyond the walls of hospitals,” explains Dr. Tsuang
The research team includes a multi-institutional and multidisciplinary team of transplant clinicians, spatial epidemiologists, statisticians, public policy experts, bioethicists and a patient investigator. “The patient investigator position is headed by a lung transplant recipient who is cared for at the Cleveland Clinic who helped inform this research application,” says Dr. Tsuang. “They are and will continue to be an integral member of the research team.”
This grant was awarded in response to a national mandate from the U.S. Department of Health and Human Services that patient geography should have a minimal role in transplant outcomes. “This is a mandate the field of transplantation has made little progress towards over the past two decades due, in large part, to gaps in knowledge that this research aims to fill,” says Dr. Tsuang. “The maps and models created will lead to an enduring framework to track the transplant field’s progress towards reducing geographic differences and improving clinical outcomes. We expect that this will be translatable and scalable throughout organ transplantation and any illness where an understanding of a patient’s neighborhood could be leveraged to improve health outcomes.”
Advertisement
Dr. Tsuang was previously awarded a five-year NIH K23 career development grant and received additional support from a Caregiver Catalyst Grant from Cleveland Clinic’s Philanthropy Institute to develop the data and collaborations necessary for this competitive and successful RO1 grant. Raed Dweik, MD, Chair of Cleveland Clinic’s Respiratory Institute notes, “Dr. Tsuang’s success is also Cleveland Clinic’s success. This work demonstrates our longstanding investment in growing the careers of clinician scientists so that we can continuously discover new ways of helping the patients of today and the patients of tomorrow.”
Advertisement
Advertisement

Milestone minimally invasive surgeries reduce pain and recovery time

Exploring the cost-effectiveness of end-of-life treatment options
Cleveland Clinic pulmonologists aim to further lower waitlist times and patient mortality

While logistical questions remain about RPM, its benefits for both patients and caregivers are abundantly clear

Long-term lung allograft outcomes clinically unaffected by organ exposure, study finds

Research explores how incorporating long-term benefits will impact the new U.S. lung transplant allocation system

Insights on ex vivo lung perfusion, dual-organ transplant, cardiac comorbidities and more

Veteran nurse blends compassion, cutting-edge transplant training and military tradition to elevate patient care