Patient selection is key
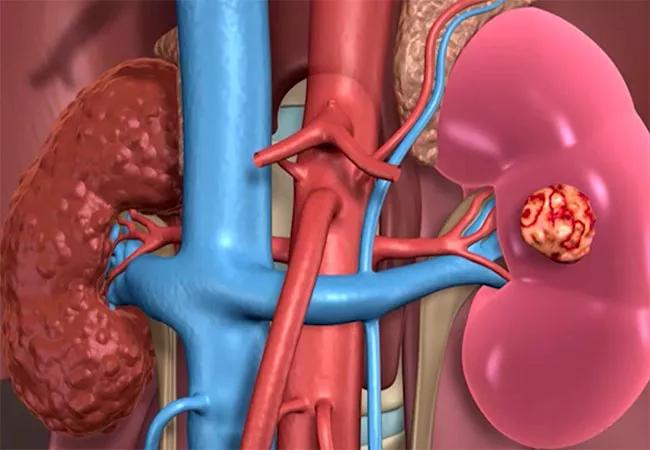
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d600b117-da24-4bdc-90c9-5f015a770b1e/650x450-Open-Partial-Nephrectomy_jpg)
650×450-Open-Partial-Nephrectomy
Alternative strategies to partial nephrectomy (PN) may lead to better outcomes for some patients with stage IV chronic kidney disease (CKD), according to a recent study in The Journal of Urology. Current guidelines recommend PN over radical nephrectomy for localized tumors in patients with CKD, proteinuria, bilateral tumors, a solitary kidney or familial kidney cancer. A team of researchers led by Steven C. Campbell, MD, PhD, of the Section of Urologic Oncology in the Glickman Urological & Kidney Institute at Cleveland Clinic, sought to determine whether the potential morbidity associated with PN is justified in all patients, and whether the procedure succeeds in its primary objective, to keep patients off of dialysis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Some patients with severe disease progress to end-stage renal disease anyway, given their comorbidities or other factors,” says Dr. Campbell. “The purpose of our study was to discover which patients might benefit from partial nephrectomy versus other approaches, like active surveillance or radical nephrectomy.”
Researchers conducted a retrospective review of all 62 patients with stage IV CKD who underwent PN at Cleveland Clinic from 1999-2015. The patients’ median age was 67 years, 84% were Caucasian and 71% were male. Most had at least one comorbidity, including hypertension (94%), cardiovascular disease (53%) and diabetes (32%). Sixteen percent of patients had benign pathology, and only 23 (37%) had tumor grade 3/4. Only 11% had pT3a disease.
Prior to surgery, the median estimated glomerular filtration rate (GFR) was 23 ml/minute/1.73 m2. Almost three-quarters of surgeries were via an open approach.
The team analyzed pre- and intraoperative factors and postoperative outcomes and determined factors associated with time-to-progression to end stage-renal disease. Fifteen (24%) patients experienced unfavorable outcomes, including 90-day mortality (3%), postoperative complication Clavien IIIb or greater (14%) or positive surgical margin (12%), confirming that this is a high-risk population.
“We also found that the median time for patients to progress to end-stage renal disease was only 27 months, and this varied according to their preoperative GFR,” notes Dr. Campbell. Patients with preoperative GFR greater than 25 ml/minute/1.73 m2 had an average of 58 months to progression, while patients with GFRs less than 20 ml/minute/1.73 m2 prior to surgery only 14 months.
Advertisement
Factors independently associated with progression to end-stage renal disease included African American race (HR 2.55 [1.10-5.95]), minimally invasive approach (HR 2.05 [1.01-4.19]) and preoperative estimated GFR 20 to 25 ml/minute/1.73 m2 (HR 2.59 [1.16-5.84]) or less than 20 ml/minute/1.73 m2 (HR 5.03 [20.3-12.4]).
This study identifies criteria that may make patients candidates for alternatives to PN, such as active surveillance or radical nephrectomy. “Our findings confirm the hypothesis that patients with pre-existing CKD are at higher risk when undergoing partial nephrectomy, and that their options need to be more carefully weighed,” says Dr. Campbell. “Improving patient selection based on factors like comorbidities, preoperative GFR and race can help us improve outcomes.”
Dr. Campbell recommends renal mass biopsy to assess oncologic risk prior to making decisions about surgical approach. Patients for whom PN would not yield significantly different outcomes may instead benefit from upfront or delayed radical nephrectomy or active surveillance.
“This is the largest study with extended follow-up of patients with stage IV CKD who underwent partial nephrectomy,” says Dr. Campbell, “and we hope that our findings allow for nuanced patient management for populations who may not receive as much benefit from partial nephrectomy as previously thought.”
Advertisement
Advertisement
Goal-of-care discussions drive earlier hospice access
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting