Guidelines weigh potential harm and benefit of breast cancer screenings, with some discrepancy among professional societies
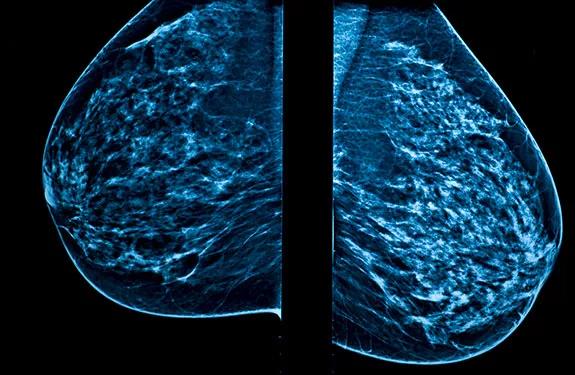
The American College of Physicians has issued new screening guidelines for women of average risk of developing breast cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The guidelines suggest that, for the average-risk woman under 50 years old who does not have breast symptoms, the potential for harm in breast cancer screenings outweigh the benefits. The guidelines emphasize the importance of beginning discussions about breast cancer risks and screening with patients at age 40. These guidelines recommend that average-risk women have mammogram screenings biennially between the ages of 50 and 74. In average-risk women who are 75 or older, with a life expectancy of 10 years or less, the recommendation is to discontinue screening for breast cancer.
Additionally, the guidelines suggest that clinical breast exams (CBE) have more potential to cause harm than benefit. Potential harms include false-positives and over-diagnosis, which may lead to over-treatment. The CBE takes 5-10 minutes to perform—time in the encounter that the American College of Physicians believes could be better used to discuss other health issues for which intervention may have more benefit.
The new statement differs slightly from guidelines set forth by the American Cancer Society, which still recommend average-risk women begin mammogram screenings at age 45 and continue them annually until age 54, and then every other year afterward.
Diagnostic radiologist Nidhi Sharma, MD, said it’s important for physicians to talk with their patients about all of available guidelines in order to help them make informed, personalized and shared decisions on when to start screening.
“In this day and age, when there are so many different guidelines, they can be confusing sometimes,” she said. “Making an informed decision is one of the most important things the patient can do for themselves, so they are screened appropriately, and the cancers are caught appropriately.”
Advertisement
The new guidelines are based on research indicating that mammograms performed every other year reduce the potential for false-positive test results, over-diagnosis, over-treatment and radiation exposure, among other factors.
But Dr. Sharma said the level of risk versus the level of benefit is different for every woman, so no guidelines are ‘one-size-fits-all.’
It’s important to note that these new guidelines do not apply to patients who have had prior abnormal screening results or who have a higher risk of breast cancer due to personal history or genetic factors. The frequency of mammography should be individualized and should involve not only an assessment of the patient’s risk factors (e.g., age, family history, genetic predisposition, history of precancerous lesions, history of radiation exposure) but also a discussion of the benefits, limitations and potential harms of screening.
Advertisement
Advertisement

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity

Psychological care can be a crucial component of medical treatment