What to look for and when to screen
By Alberto J. Montero, MD, MBA
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Primary care physicians play a vital role in detecting cancers at earlier stages and synthesizing information from a patient’s presentation, vital signs, physical examination and results of laboratory and radiographic testing. This post provides clinically relevant breast cancer pearls from an oncologic perspective for primary care physicians.
Breast cancer is the second most common cause of cancer death in US women and the most common cause of death in US women ages 20 to 59.
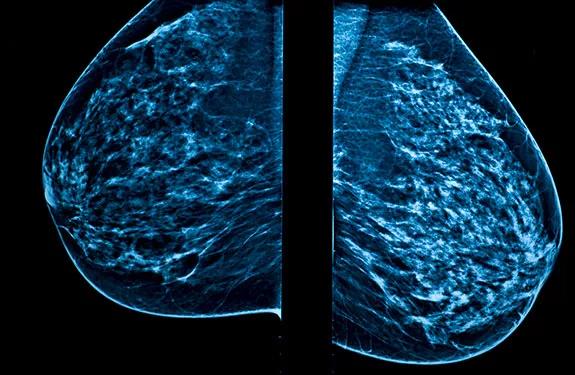
Screening mammography has had a significant impact on early detection rates, and this has translated into a 20 to 30 percent decrease in the breast cancer mortality rate. But despite national screening guidelines, up to 15 percent of cases are diagnosed on the basis of a palpable breast mass not detected on mammography, and 30 percent are diagnosed with a breast mass during the interval between mammograms.
Breast cancer can present clinically as a single, dominant, indurated mass with irregular borders. The mass can have associated ecchymosis, erythema, nipple discharge, nipple retraction and nipple eczema. Pay close attention to any history of breast trauma, pain, signs or symptoms suggestive of local infection, and the lesion’s relationship to the patient’s menstrual cycle. Locally advanced disease typically presents with axillary adenopathy, as well as skin findings such as erythema, thickening and dimpling.
Women presenting with a breast mass should undergo breast imaging, followed by core needle biopsy of any suspicious abnormality. Depending on the clinical breast examination and the interpretation of the mammogram, as reported as a Breast Imaging Reporting and Data System (BIRADS) score, ultrasonography, magnetic resonance imaging or biopsy may be the next course of action. Ultrasonography is recommended in evaluating masses in women who are under age 30 (who are more likely to have dense breasts that make standard mammography difficult to interpret) or who are pregnant (because it does not involve radiation).
Advertisement
For patients with a borderline or indeterminate clinical examination (e.g., asymmetric skin-thickening or discoloration, nipple discharge or inversion, nodularity, finding on imaging [i.e., BIRADS 3 lesion]), closer follow-up with repeat or additional imaging or biopsy, or both, is strongly recommended.
The age at which to start breast cancer screening has been a matter of debate in recent years, and different organizations have different recommendations. According to the American Cancer Society (ACS), women should begin screening mammography at age 45 and should continue it indefinitely as long as they are in good health. This guideline is in line with those of the National Comprehensive Cancer Network (NCCN) but differs from those of the U.S. Preventive Services Task Force (USPSTF).
One reason for the controversy is that although starting screening at a younger age may allow for earlier detection, it also leads to overdiagnosis and to unnecessary tests and procedures. However, the NCCN noted limitations in studies looking at the overdiagnosis of breast cancer, including their use of incidence data from the 1970s, which not only underestimated the annual incidence of breast cancer in the United States, but also neglected to differentiate invasive cancer from ductal carcinoma in situ. Additionally, by detecting breast cancer lesions two years before they are discovered by clinical breast examination, mammography has been found to reduce the mortality rate from breast cancer.
Advertisement
The frequency of mammography should be individualized and should involve not only an assessment of the patient’s risk factors (e.g., age, family history, genetic predisposition, history of precancerous lesions, history of radiation exposure) but also a discussion of the benefits, limitations and potential harms of screening. Both the ACS and the NCCN recommend yearly mammography for women ages 45 to 54. For those age 55 and older, the ACS recommends screening mammography every two years until the patient’s life expectancy is less than 10 years, whereas the NCCN recommends yearly screening mammography indefinitely. Meanwhile, the USPSTF recommends mammograms every two years for women ages 50 to 74.
Dr. Montero is staff in the Department of Solid Tumor Oncology.
This post is adapted from and contains part of an article that originally appeared in Cleveland Clinic Journal of Medicine. Read the full article for pearls on other types of cancer.
Advertisement
Advertisement

Emerging evidence suggests a patient-specific approach

Not if they meet at least one criterion for presumptive evidence of immunity

Essential prescribing tips for patients with sulfonamide allergies

Confounding symptoms and a complex medical history prove diagnostically challenging

An updated review of risk factors, management and treatment considerations

OMT may be right for some with Graves’ eye disease

Perserverance may depend on several specifics, including medication type, insurance coverage and medium-term weight loss

Abstinence from combustibles, dependence on vaping