Research reveals that diverting ostomy is also not a stricturing factor
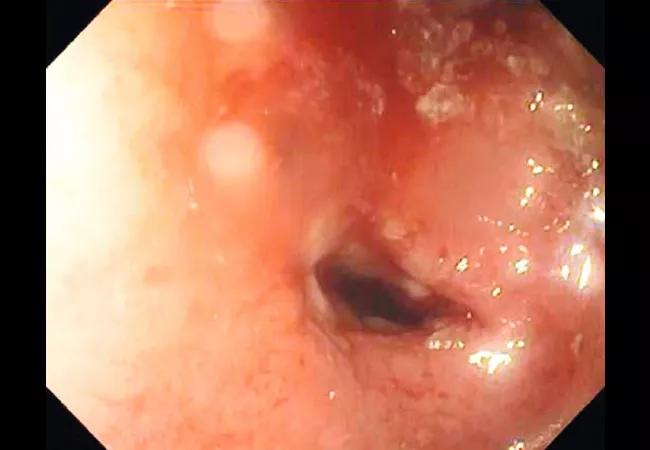
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e84c5c18-be59-430a-b0e1-9b2903fc8a75/18-DDI-5583-Shen-Hero-Image-650x450pxl_02_jpg)
18-DDI-5583-Shen-Hero-Image-650x450pxl_02
The risk of strictures following ileocecal resection for Crohn’s disease (CD) doesn’t appear to be influenced by the surgical approach to anastomosis or the use of a diverting ostomy, new research suggests.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Anastomotic and neoterminal ileal strictures are known consequences of CD recurrence following ileocolonic resection. Until now, little had been known regarding the role of anastomotic configuration in stricture formation, although some researchers had hypothesized that diverting ostomies or certain types of primary anastomoses might increase the stricture risk.
This new study refutes that premise.
“Simply put, we found that neither one influenced that risk. These are new findings in our field from a medical and surgical standpoint,” says study co-author Miguel Regueiro, MD, Chair of Cleveland Clinic’s Digestive Disease & Surgery Institute.
The results, Dr. Regueiro says, “reassure us that when a patient needs a temporary diverting ileostomy to allow for healing of infection and inflammation around the anastomosis, that’s OK since there is not a higher rate of stricture. And, if the surgeon’s preference is to do the anastomosis either end-to-end, side-to-side, or end-to-side, there’s no real difference between those in terms of the stricturing rates after surgery.”
Cleveland Clinic internal medicine resident Muhammad Zarrar Khan, MD, a coauthor of the study, presented the findings at the 2022 Digestive Disease Week annual meeting.
The study involved 606 patients who underwent ileocecal resection for CD between 2009 and 2020 and who also underwent postoperative ileocolonoscopy. The procedures took place at three centers of expertise in colorectal surgery: Cleveland Clinic, the University of North Carolina (UNC) Chapel Hill, and New York University (NYU) School of Medicine. More than half of the patients were seen at Cleveland Clinic.
Advertisement
The patients had a median age at surgery of 34.5 years, just under half (47.5%) were male, and 41% were smokers — a factor believed to increase the risk for CD recurrence and strictures. About one in five was started on postoperative biologic prophylaxis.
A majority (n=426, or 70.3%) had a primary anastomosis at the time of resection, including 78 end-to-end, 117 end-to-side and 231 side-to-side. The rest had either diverting loop ileostomy (22.8%) or end ileostomy (6.9%).
Anastomotic strictures developed in a total of 18.2% of the 606 patients at a median time of 1,207.5 days post-surgery. 18.8% of the strictures occurred in patients with end-to-end anastomoses, 20.3% end-to-side and 16.8 side-to-side.
Survival analysis showed that anastomotic configuration was not associated with stricture formation (p=0.098), even after controlling for the postoperative recurrence risk factors of biologic prophylaxis and use of a diverting ostomy.
This result was somewhat unexpected, since it had been thought that the end-to-end configuration might increase the risk for stricture because the inner diameter it creates is smaller than the other two types. “But this study did not show that,” Dr. Regueiro notes.
Moreover, compared to primary anastomosis, there was no difference in stricture formation for those receiving diverting loop (adjusted hazard ratio 1.36, p=0.19) or end ileostomy (0.35, p=0.14). This, too, was a bit of a surprise. “I was kind of expecting that diverting ostomies would ultimately develop more strictures after reconnection of the bowel. That had always been the theory,” Dr. Regueiro says.
Advertisement
Ongoing studies at Cleveland Clinic, some also in collaboration with UNC and NYU, are investigating the optimal surgeries and medications to prevent CD recurrence. Cleveland Clinic’s colorectal surgery program is the largest in the country, comprising 27 surgeons who operate on about 10,000 patients with inflammatory bowel disease annually.
The research’s bottom line is that the choice of which anastomotic configuration to use and whether to employ a diverting ostomy should be guided by the surgeon’s experience and the patient’s individual requirements.
According to Dr. Regueiro, “This was a great study for us in the field going forward. We didn’t see differences in strictures and blockage, which I think is really important. The take-home message is do the right surgery for the patient, including diverting ostomy, if required.”
Advertisement
Advertisement
Benefits of neoadjuvant immunotherapy reflect emerging standard of care
Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence
Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors
Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling
Potentially cost-effective addition to standard GERD management in post-transplant patients
Findings could help clinicians make more informed decisions about medication recommendations
Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care
Retrospective analysis looks at data from more than 5000 patients across 40 years