Nationwide research underscores the importance of individualized treatment

A nationwide research effort — conducted in collaboration with Cleveland Clinic — underscores the high risk of postoperative recurrence among older adults with Crohn’s disease following ileocolic resection (ICR). This data, recently presented during the Digestive Disease Week conference, also demonstrates that while biologic prophylaxis significantly reduces the risk of both endoscopic and composite recurrence, it is less frequently administered to older patients.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“These findings emphasize the importance of prioritizing individualized treatment tailored to the disease and patient, rather than focusing solely on chronological age,” notes study author Miguel Regueiro, MD, Chief, Digestive Disease Institute at Cleveland Clinic.
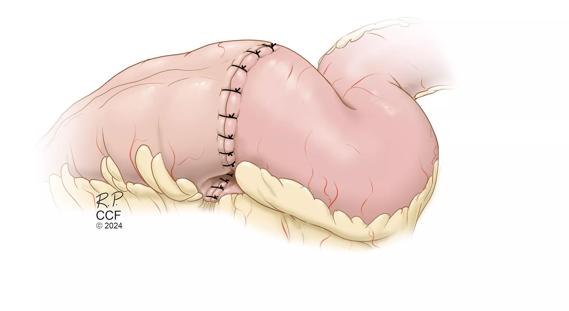
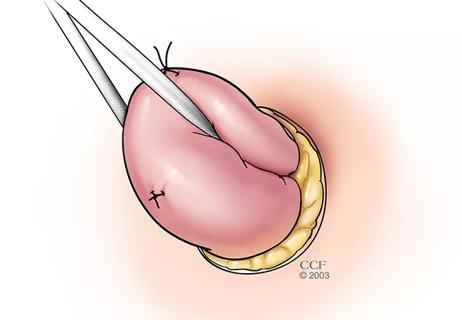
Postoperative recurrence (POR) after ileocolic resection is common in Crohn’s disease; however, limited data exist on recurrence rates and associated risk factors, specifically for older adults. Dr. Regueiro, prompted by a deep interest in postoperative management of Crohn’s disease and a desire to improve outcomes in this patient population, collaborated with colleagues across the country to examine how age influences the risk of postoperative recurrence as well as associated risk factors.
This multicenter, retrospective study included patients with Crohn’s disease who underwent ileocolic resection between 2009 and 2020. The cohort was divided into two groups: older patients (≥60 years) and younger patients (18–59 years). Among the 1,095 participants, 86.8% were younger and 13.2% were in the older patient cohort.
Researchers evaluated POR-free survival at 1-, 3-, and 5-year follow-up intervals as well as the association between selected risk factors, such as age, tobacco history, perianal disease, and post-operative biologic prophylaxis with postoperative recurrence risk.
In this analysis, postoperative was defined as endoscopic (Rutgeerts’ score ≥ i2b), radiologic (inflammation on imaging), surgical (redo ICR), or composite (endoscopic, radiologic, or surgical) recurrence.
Advertisement
“This study represents the largest cohort of Crohn’s disease patients evaluated after surgery,” Dr. Regueiro notes. “With a total of 1,095 Crohn's patients who have undergone surgery, we have a rich pool of data to explore. Although the study is retrospective, the large dataset still makes it valuable from a methodological perspective.”
Key findings from the study include the following:
“Compared to younger patients, older age was associated with a significantly shorter time to composite POR when evaluating at the 5-year follow-up interval, largely driven by higher endoscopic POR rates in older patients,” Dr. Regueiro and colleagues report.
Data revealed that initiation of biologic prophylaxis within 90 days of surgery was associated with significant risk reduction in both endoscopic and composite postoperative recurrence at all time intervals. Additionally, no significant difference in surgical POR was observed between the two age groups. In older patients, biologic prophylaxis was associated with a significantly longer time to composite POR at the 5-year follow-up interval.
Advertisement
Historically, biologic therapies have been used less frequently among older patients with inflammatory bowel disease, such as those with Crohn’s disease, due to concerns regarding potential risks. This new analysis highlights the importance of moving beyond chronological age as a sole factor in treatment decisions and emphasizes the need for individualized care that takes into account each patient's unique health status and risk for recurrence.
This research sheds further light on the heightened risk older adults with Crohn’s disease face regarding postoperative recurrence, especially after ileocolic resection. It also illustrates the crucial role of biologic prophylaxis in preventing recurrence, yet also points to a gap in treatment—older patients are less likely to receive biologic therapy despite its proven benefits.
“We cannot treat age as just a number. We need to consider the patient’s overall health and adjust our clinical decision-making accordingly,” Dr. Regueiro concludes. “Our findings emphasize the importance of considering age- and disease-specific treatment strategies as well as suggest that biologic prophylaxis should be considered for older patients at high risk of recurrence, as it could significantly reduce the likelihood of postoperative recurrence and improve long-term outcomes.”
Ultimately, this study advocates for a more individualized, patient-centered approach to the management of postoperative Crohn’s disease, one that ensures all patients, regardless of age, receive the most appropriate care for their specific needs.
Advertisement
DDW Presentation: “Older Patients with Crohn’s Disease Remain at High Risk for Postoperative Recurrence and Benefit from Medical Prophylaxis”
Advertisement
Advertisement

Study utilizes prospective data from the RISK cohort
Findings support the safety of the technique

Strong patient communication can help clinicians choose the best treatment option
Findings from a 2023 ASCRS presentation indicate that both 2-stage and modified 2-stage approaches are viable management strategies for Crohn’s patients who require a temporary ileostomy

New research identifies a direct functional link between creeping fat and muscle

Retrospective analysis looks at data from more than 5000 patients across 40 years

The Integrated Program aligns IBD care and research across Cleveland Clinic locations

Diet has a profound impact on how the intestine functions