Study results highlight need for surveillance, education
Patients with inflammatory conditions and concomitant cirrhosis who are treated with tumor necrosis factor (TNF) inhibitors face heightened risk of serious infections and other complications, according to Cleveland Clinic research presented at the Digestive Disease Week 2019 annual meeting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“While the results of our retrospective multicenter study do not preclude the use of anti-TNF drugs in cirrhotic patients, they highlight the need for caution in treatment planning,” explains principal investigator Jamak Modaresi Esfeh, MD, of the Digestive Disease & Surgery Institute’s Department of Gastroenterology and Hepatology. “They also emphasize the need for vigilant surveillance, as well as physician and patient education.”
TNF inhibitors are a category of biologic agents that have become important in the treatment of autoimmune inflammatory conditions such as rheumatoid arthritis, inflammatory bowel disease and psoriasis. Anti-TNF agents suppress the potent pro-inflammatory cytokine TNF-α and thereby reduce chronic pathologic inflammatory responses.
However, TNF inhibitors pose a risk of serious opportunistic infections and/or cancer because of their immunomodulatory affects. “Due to their high potency and infection risk, physicians usually recommend them as a second- or third-line medication, when first-line medications prove ineffective,” Dr. Esfeh says.
Inflammatory diseases may be comorbid with cirrhosis, an immunocompromising condition that predisposes patients to infections as well as hepatic and extra-hepatic malignancies and other complications. Infections can lead to acute-on-chronic liver failure. There is concern — and limited information in the medical literature — about TNF inhibitors’ potential to compound existing infection/cancer risks and cause hepatic decompensation in patients with co-occurring inflammatory disease and cirrhosis.
Advertisement
In 2018, Dr. Esfeh and colleagues evaluated the use of the relatively new biologic drug vedolizumab in a small cohort of patients with concomitant Crohn’s disease and cirrhosis and determined that there were no episodes of hepatic decompensation, significant infections or malignancies after months of treatment.
The latest research builds on those results. It is the largest known study to date assessing the safety of anti-TNF agents in cirrhotic patients. Dr. Esfeh collaborated with co-principal investigator Nikhil Kapila, MD, a gastroenterology fellow at Cleveland Clinic Florida.
The researchers retrospectively evaluated the medical records of 98 patients with a variety of inflammatory conditions and concomitant cirrhosis who were treated with TNF inhibitors. The most common condition for anti-TNF use was psoriatic arthritis (38.2%) and the most commonly prescribed TNF inhibitor was adalimumab (58.2%). Average treatment duration was 5.6 years. The study’s primary end-point was hepatic decompensation as evidenced by ascites, esophageal varices or hepatic encephalopathy. Secondary end-points were serious infection or hepatic or extra-hepatic malignancies.
A total of 56 patients (57.1%) decompensated during treatment. Seventeen (18.1%) developed serious infections. Four (4.2%) developed hepatocellular carcinomas and six (6.1%) were diagnosed with extra-hepatic malignancies. The incidence of serious infections in the study cohort was higher than historical rates of serious infections in non-cirrhotic patients treated with TNF inhibitors. The incidence of hepatic and extra-hepatic cancers in the anti-TNF cohort was comparable to what is expected in the natural course of cirrhosis.
Advertisement
The results indicate that anti-TNF therapy is safe to use in cirrhotic patients. However, they reinforce the need for caution as well as patient and physician education about potential risks.
“Although cirrhotic patients had a higher risk of infection, the results are not a contraindication for use,” explains Dr. Esfeh. “Instead, physicians must be vigilant if an infection develops, educating patients about the need to immediately report infection-related symptoms such as fever or chills.” Vigilance is vital because infections that progress in cirrhotic patients could lead to acute-on-chronic liver failure.
Further research is needed to assess the long-term outcomes for patients who develop infections during anti-TNF treatment. Additionally, there is a need to evaluate the amount and severity of anti-TNF-related complications in patients with elevated Model for End-Stage Liver Disease (MELD) and Child-Pugh scores. Clinicians use the MELD and Child-Pugh scoring systems to assess the severity of patients’ cirrhosis.
“Studying larger patient populations with these higher scores will allow us to make clearer treatment recommendations for patients with severely compromised liver health,” says Dr. Esfeh.
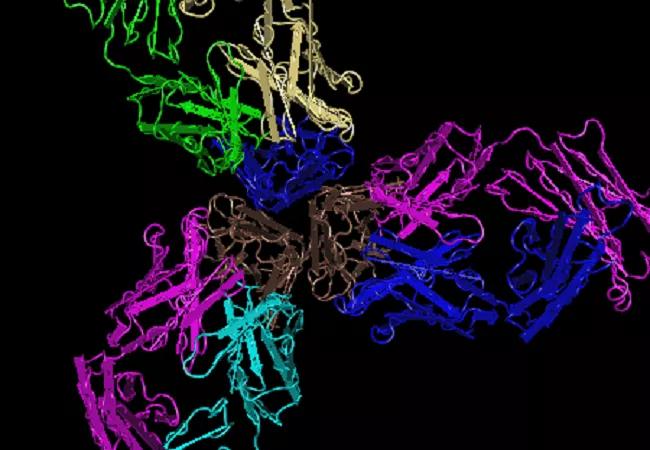
3-D molecular image of the crystal structure of TNFα in complex with the anti-TNF agent infliximab Fab. Credit: National Center for Biotechnology Information.
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years