Study reports zero infections in nearly 300 patients
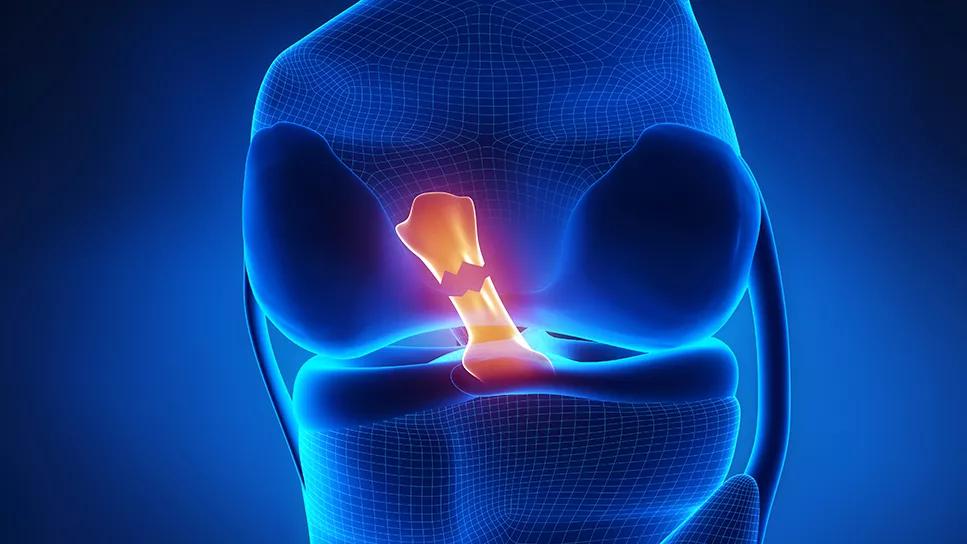
Cleveland Clinic orthopaedic surgeon Kurt P. Spindler, MD, is on a mission to document that aspiration and corticosteroid injection in the knee is safe and beneficial for young, healthy patients following anterior cruciate ligament (ACL) rupture and before reconstructive surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Despite growing evidence that knee aspiration and corticosteroid injection reduce the risk for post-traumatic osteoarthritis (PTOA) following ACL rupture, many surgeons are reluctant to perform them due to fear of infection.
“The underlying feeling in orthopaedics is that corticosteroids are bad, that they increase the infection rate,” says Dr. Spindler, Director of Clinical Research and Outcomes at Cleveland Clinic Florida. “I believed that my patients hadn’t had any infections, so I decided to document it to show that concerns about corticosteroids were unfounded.”
He and his colleagues recently published a retrospective study in The American Journal of Sports Medicine, showing that over a 10-year period there were zero infections in 693 consecutive patients who underwent ACL reconstruction, including 273 who received aspiration and injection after the ACL rupture but before the surgery.
“That’s what research is about, trying to document what exists and what doesn’t exist. In my population, infection due to aspiration and injection did not occur,” says Dr. Spindler, who served as the 2021-2022 President of the American Orthopaedic Society for Sports Medicine.
Importantly, individuals evaluated in the study were between ages 10 and 65, with a median age of 26 for those who received the aspiration/injection. Thus, they were younger and healthier than cohorts in previous studies of joint replacement, which included older patients who already had an advanced degree of arthritis. In older populations with existing arthritis there is a link between corticosteroid injection and subsequent infection — although only a small percentage increase, notes Dr. Spindler.
Advertisement
In the current study, the group that didn’t receive aspiration/injection was slightly older (28 vs. 25.6 years, P = .014). The aspiration/injection group had a significantly shorter mean time from injury to office visit (9.4 vs. 231.8 days, P < .001), with most of the aspiration/injection procedures carried out on that first visit.
The mean time from initial office visit to surgery didn’t differ significantly between the groups (63.3 days with aspiration/injection vs. 82.2 days without, P = .348), but the aspiration/injection group had a longer mean follow-up time (351.3 vs. 328.3 days, P = .002).
This study follows a 2016 multicenter trial comparing corticosteroid with placebo injections at four days or two weeks following ACL injury in relatively young and healthy patients. No adverse events or infections occurred in any study participants, and there were no differences in patient-reported outcomes, including pain.
However, the placebo group showed greater subsequent breakdowns in collagen and decreases in cartilage oligomeric matrix protein compared with those who received corticosteroid injections, suggesting corticosteroid may have protective properties for the articular cartilage.
“These findings can’t be extrapolated beyond the young knee injury population that doesn’t have any pre-existing arthritis and that has a bloody effusion,” emphasizes Dr. Spindler, senior author of the 2016 study. “However, the study shows that, in this population, corticosteroid injection is safe.”
Advertisement
Going forward, the challenge will be to identify a second agent to be used after ACL reconstruction to reduce further PTOA risk incurred from the surgery.
“When you do surgery on the knee and rinse out all the lubricating factors, including lubricin and hyaluronic acid that protect the cartilage, you also create a very large hemarthrosis [bloody effusion],” says Dr. Spindler. “In addition, you create particle debris in the joint from bone and soft tissue. That’s multiple injuries.”
Unlike the presurgical intervention to block inflammation, an agent used post-surgery would need to also allow healing.
“Healing and inflammation are so tightly coupled that if you just block inflammation, it may destroy the healing for which you performed the reconstruction,” he explains. “There needs to be a different agent to inject after surgery that does not have a negative effect on healing. We don’t have that right now. A lot of people are thinking about it, but it’s very early in development.”
Meanwhile, Dr. Spindler says the data from his 2023 study should help surgeons feel confident that aspirating and injecting corticosteroid into the knee of a young athlete with a torn ACL will not harm them and may well help.
“I think if you have an acute bloody effusion of the knee, you should sterilely aspirate it, inject cortisone prior to surgery and get the patient rehabbed faster,” concludes Dr. Spindler.
Advertisement
Advertisement

Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction

Self-care may be just as effective for some patients

Most return to the same sport at the same level of intensity

Higher than 5-year rates for prostate cancer and melanoma and about the same as breast cancer

Insights to help orthopaedic practices comply with the 2025 CMS mandate

Dr. Piuzzi wins 2025 Kappa Delta Young Investigator Award for pioneering work

Largest cohorts to date reveal low rates of major complications

Growth modulation procedures are effective if the condition is diagnosed before the patient reaches skeletal maturity