Q&A with newly arrived autoimmune neurology specialist Amy Kunchok, MD
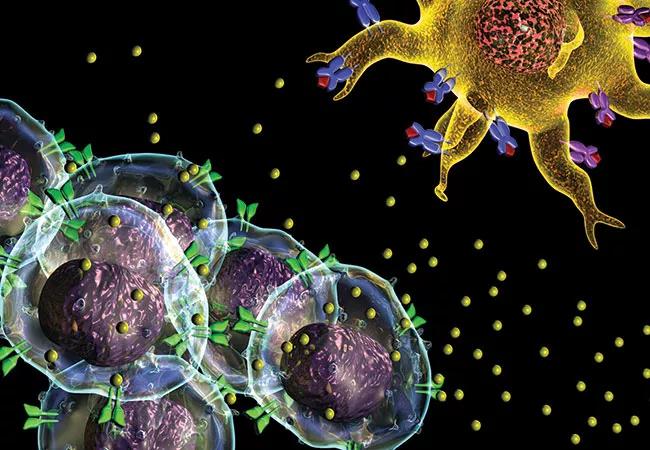
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/30e404c0-4daf-4790-b1cc-72acef9405e6/20-NEU-2020111-neuroimmunology_650x450_jpg)
20-NEU-2020111 neuroimmunology_650x450
Autoimmune encephalitis and other autoimmune neurologic disorders are increasingly identified causes of unexplained dementia and other neurologic symptoms. Their prompt recognition is important, as these disorders can often be successfully treated with steroids or more specific immunotherapies before permanent neurologic damage develops.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Disorders of this type are the specialty of Amy Kunchok, MD, MBBS, one of the newest staff appointed to Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research. Dr. Kunchok took on her new post in mid-2020 after fellowships in multiple sclerosis and autoimmune neurology at the Mayo Clinic following training in internal medicine and neurology in her native Australia.
Consult QD recently asked Dr. Kunchok about the rapidly advancing subspecialty of autoimmune neurology and some of the related program offerings she brings to the Mellen Center.
Dr. Kunchok: For autoimmune encephalitis, great advances have been made in the past 20 years in recognizing clinical phenotypes and their associated autoantibody biomarkers. Novel biomarkers are still being discovered, including the recently identified PDE10A-IgG in patients with movement disorders and KLKH11-IgG in males with testicular cancer and brainstem-cerebellar symptoms.
We also have developed a greater understanding of the pathogenesis of many of these disorders. We now understand that a proportion of NMDAR-IgG encephalitis occurs after herpes simplex virus encephalitis, suggesting post-viral-induced autoimmunity. HLA associations have suggested distinct immunogenetic pathways in in LGI1-IgG and CASPR2-IgG encephalitis. In addition, we are gaining a better understanding of how biological therapies such as immune checkpoint inhibitors work, providing important insights into the development of central nervous system autoimmunity.
Advertisement
We’ve likewise seen great strides in the field of neuromyelitis optica spectrum disorder (NMOSD). Randomized clinical trials have been completed for three new immunotherapies, showing good efficacy. These will lead to better management of NMOSD, with the goal of fewer relapses and less disability.
Other central nervous system disorders, including myelin oligodendrocyte glycoprotein (MOG-IgG1) disorders, are increasingly recognized. These MOG-IgG1-associated disorders can have clinical findings of acute disseminated encephalomyelitis (ADEM), optic neuritis, myelitis and encephalitis. Research is continuing in this area in an effort to characterize clinical, radiological and serological features of these disorders, as well as clinical outcomes and response to immunotherapies.
Dr. Kunchok: There is much greater recognition now of autoimmune encephalitis, particularly in the settings of status epilepticus and new onset of marked neurocognitive or neuropsychiatric changes. But for patients with more subtle abnormalities — such as mild to moderate cognitive changes, seizure auras and faciobrachial seizures — an autoimmune cause is often overlooked.
Dr. Kunchok: I am especially interested in autoimmune and paraneoplastic encephalitis as well as atypical demyelinating disorders, including NMOSD and MOG-IgG1-associated disorders. I am developing an integrated autoimmune neurological data registry at Cleveland Clinic to prospectively collect clinical, radiological and serological data on our patients, which we expect will be extremely useful for future research.
Advertisement
Dr. Kunchok: Tumor necrosis factor (TNF)-alpha inhibitors were among the earliest monoclonal antibodies developed as therapies for autoimmune disorders and are highly effective. However, in some patients we found they were associated with atypical inflammatory central nervous system events, including demyelination and meningitis/meningoencephalitis. When assessing patients with such events, it is important for clinicians to consider medication history and specifically whether they have had exposure to therapies such as TNF-alpha inhibitors.
Dr. Kunchok: The Mellen Center has a history of providing comprehensive clinical care for patients with complex neuroimmunologic conditions. We have now formalized and expanded this to focus on autoimmune/paraneoplastic encephalitis in addition to NMOSD and MOG-IgG1-associated disorders.
The comprehensive data registry I mentioned before will enable patients to contribute to future observational clinical research simply by participating in their own routine comprehensive care. The goals of such studies are to help predict clinical outcomes and how to choose optimal therapy for these diseases. We will also provide patients the opportunity to participate in the latest clinical trials as they get underway.
Advertisement
Advertisement
A case study in pairing imaging acumen with subspecialty expertise to yield answers and symptom relief
Guidance from the largest cohort of SEEG-confirmed insular epilepsy patients reported to date
Ethical guidance provides guardrails so medical advances benefit patients
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
An argument for clarifying the nomenclature
An expert talks through the benefits, limits and unresolved questions of an evolving technology