Q&A with Brain Trauma Foundation guideline architect Gregory Hawryluk, MD, PhD
Neurosurgeon Gregory Hawryluk, MD, PhD, recently joined the Level I Trauma Center at Cleveland Clinic Akron General Hospital. Dr. Hawryluk has been instrumental in shaping guidelines for the management of severe traumatic brain injury (TBI) through his role as Medical Director and Chair of the Scientific Advisory Board of the Brain Trauma Foundation (BTF), the preeminent guideline-setting organization for brain trauma.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
ConsultQD recently caught up with Dr. Hawryluk to discuss current issues and challenges in neurotrauma management, along with what the field might expect next.
Q: How do neurosurgeons keep updated on best standards of practice for brain trauma?
A: The BTF website is a great resource for current head injury guidelines. They have been created on a range of important subtopics related to severe brain trauma in both adults and children, including prehospital management, prognostic indicators, coma, concussion, surgical management and field management in combat settings.
The use of these guidelines — which have been developed, expanded, updated and refined by the BTF over more than 25 years — is consistently associated with a 50% reduction in mortality, as well as reduced costs of patient care. The early guidelines represented a significant advance for the field by recommending against harmful practices common at the time, such as hyperventilation, steroid administration and inadequate resuscitation due to fear of causing brain edema.
BTF guidelines are respected and used around the world in a variety of settings, and accreditation of American trauma centers now relies heavily on compliance with them. The secret to the guidelines’ success is our rigorous methodology. The BTF’s evidence-based recommendations have earned the trust and respect of physicians worldwide. And although the guidelines have literally saved millions of lives, there remain centers where they are underused.
Q: Why is that?
Advertisement
A: Evidence-based guidelines can only get us so far. We have been criticized for not making them practical enough for a variety of real-world settings. Of course, we are limited by lack of evidence in many cases. To help address this concern, we are looking to the algorithm-development model used by the Seattle International Severe TBI Consensus Conference (SIBICC). For future guideline publications, the BTF is endeavoring to generate algorithms based on the evidence we have, but with the addition of expert opinion to bridge the gaps.
[Editor’s note: Dr. Hawryluk co-chaired the SIBICC and led the development of two important algorithms for TBI patients published in Intensive Care Medicine, one based on intracranial pressure (ICP) monitoring and the other on both ICP and brain oxygen monitoring.]
Q: What are important trends in research now?
A: Head injury is a particularly difficult topic to study, and good evidence is scarce. Of course, trauma arises in an emergency, making traditional clinical research design more challenging.
The one thing that has been demonstrated to help TBI outcomes is supportive care. A lot of ongoing work seeks to optimize this supportive care. Central to this has been the maintenance of certain thresholds like brain pressure and blood pressure. Whether we are using the best thresholds is an active research topic. I think, though, that a key question is whether we should actually be looking beyond simple thresholds that involve a single number for all patients. [Editor’s note: See Dr. Hawryluk’s recent reviews of intracranial pressure management research in Current Opinion in Critical Care and Intensive Care Medicine.]
Advertisement
I think it is also becoming increasingly apparent that the field may have overlooked some fundamental issues and has been slow to advance because of that. Until recently we haven’t sufficiently considered phenomena termed cortical spreading depolarizations. We also haven’t sufficiently considered cerebral autoregulatory phenomena and their relationship to cerebral blood volume in contributing to brain pressure changes.
I have a special interest in the area of autoimmunity following brain injury. This line of investigation could potentially advance our understanding of chronic traumatic encephalopathy and lead to the development of preventive, targeted anti-inflammatory therapies. [Editor’s note: See Dr. Hawryluk’s recent research in this area in Neuroscience Research.]
Q: You also have a professorship with the federal government’s Uniformed Services University. Does experience with head trauma in the military inform civilian management?
A: Definitely. Although civilian doctors have the advantage of more dependable resources and a more controlled environment, no one in the civilian world sees as many cases of severe, complex and penetrating head trauma as physicians working in war zones. This sets the stage for a very productive two-way street of information sharing. The U.S. Department of Defense (DoD) and the BTF have embarked on multiple collaborations to perform mutually beneficial projects. With the help of DoD funding, the BTF for the first time is conducting its own research to fill critical knowledge gaps, including investigating the potential role of early lumbar cerebrospinal fluid drainage to avert intracranial hypertension.
Advertisement
As a result of the DoD-BTF collaboration, in the coming years we can look forward to new TBI guidelines for combat settings and austere environments, as well as new concussion guidelines — including when to return to combat or sport. We will also be updating our flagship adult severe TBI guidelines, which are currently in their fourth edition.
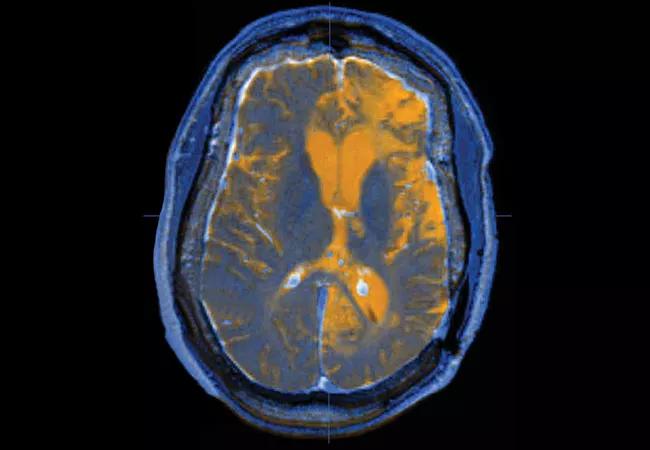
Image at top: Axial image of a patient with traumatic brain injury created by fusing T1 and T2 MRI data sets.
Advertisement
Advertisement

New guidance on penetrating head injuries, and noninvasive diagnostics get a nod in austere settings

New guidelines from Brain Trauma Foundation urge early and aggressive treatment

Machine learning study associates discrete neuropsychological testing profiles with neurodegeneration

Exploring new tools and techniques to improve the diagnosis and treatment of concussions.

Training, tools and resources lead to safer, more compassionate care

Promising preclinical research indicates functional motor recovery is durable

Cleveland Clinic researchers collaborate with Microsoft to create a product ready for the field
New research sheds light on a potentially devastating condition that is reversible when properly managed