Q&A with writing group vice chair Mina Chung, MD
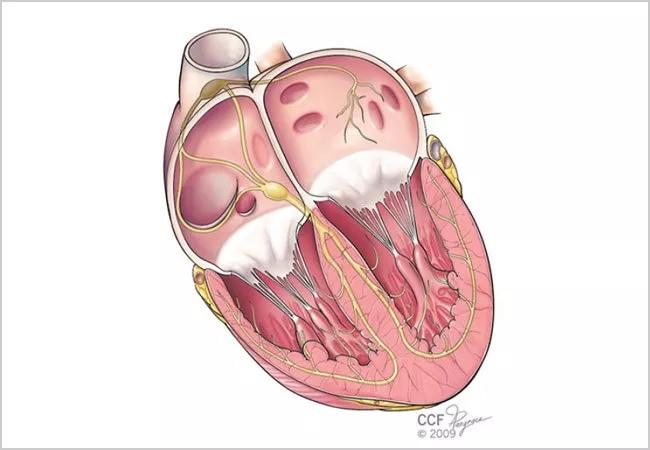
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/dd06f23a-2c5b-4a6d-a156-1aa90e17fc7c/18-HRT-4534_Chung_atrial-fibrillation_650x450_jpg)
Beyond the Binary in Atrial Fibrillation: AHA Statement Calls for Focus on AF Burden
Atrial fibrillation (AF) is typically defined by type or pattern — paroxysmal versus nonparoxysmal, or persistent versus permanent — but it can also be looked at quantitatively. AF burden is a measure of the amount of AF a person has, in terms of duration of AF episodes, number of episodes or the percentage of time the person is in AF.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Noting that current understanding of AF risk factors and complications is based largely on studies that have not investigated AF burden, the American Heart Association (AHA) recently convened a writing group to develop a scientific statement on AF burden. The statement, published in Circulation in April, synthesizes pertinent research and calls for more nuanced definitions and AF treatment protocols.
Cleveland Clinic electrophysiologist Mina Chung, MD, served as vice chair of the writing group, so Consult QD asked her what clinicians need to know about the new statement.
Q: Why was this statement developed?
A: Existing guidelines about AF have generally treated AF in binary fashion: You either have AF or you don’t. We wanted to examine the literature to see if higher AF burden is associated with worse outcomes and how that relationship tracks along a continuum of severity. We also wanted to learn more about how lifestyle decisions relate to AF burden. We suggest that a nuanced appreciation of degrees of AF burden will be most useful in guiding treatment.
Q: Why does a more nuanced understanding of AF burden matter?
A: Higher AF burden is associated with higher risk of stroke, heart failure and mortality, and treatment for more persistent AF leans toward more aggressive therapy, including anticoagulation, antiarrhythmic drugs or ablation approaches. But aggressive therapies carry their own risks, of course. Recent evidence suggests that painting with a broad brush may not be ideal and that outcomes for patients with paroxysmal AF, for example, may not warrant the same therapy as for those with more persistent, long-standing persistent or permanent nonparoxysmal AF.
Advertisement
There are questions on which we need some consensus. For instance, current guidelines recommend using usual risk-scoring systems, such as the CHA2DS2-VASc score, to make recommendations on anticoagulation in patients with AF. However, in patients without overt clinical AF, what’s the threshold of AF burden that justifies anticoagulation therapy? This issue arises frequently in patients with pacemakers or defibrillators that detect AF.
Q: What are some takeaways from the literature reviewed for this statement?
A: One important takeaway is that there’s strong evidence that a structured and comprehensive program that targets risk factors may reduce AF burden as well.
Another is how highly concordant heart failure and AF are. AF occurs in more than half of patients with heart failure, and heart failure occurs in more than a third of people with AF. Beyond stroke risk, this further underscores the need for early, appropriate AF intervention.
Q: Where are some key knowledge gaps, and how can we fill them?
A: We need to learn much more about the existence and significance of the thresholds I mentioned and which interventions might reduce AF burden, improve quality of life and reduce stroke risk. New monitoring technologies will be important tools in this research.
Also, we don’t really understand the relationship between degrees of AF burden and cognitive performance. One small study pointed to greater cognitive risk with persistent versus paroxysmal AF, but the research is sparse. Additional studies are needed to better understand this relationship.
Advertisement
Q: Did anything particularly stand out for you?
A: I was surprised that the relationships between higher AF burden and higher stroke risk or cognitive function are not as well-characterized as they could be. We know, through data collected from implantable devices, that some short episodes of AF can be associated with higher risk, but we don’t know whether this is a continually increasing risk or if there’s a threshold beyond which the risk surges.
Some clinicians may be surprised how weak the temporal relationship is between AF episodes and stroke. This is something learned from studies using time-stamped device data. So an atrial clot that forms may or may not always be due to a preceding or current episode of AF. This raises questions about the origins of thrombotic formation in the heart, suggesting that AF might be a marker of an atrial myopathy or a milieu that predisposes to both AF and stroke. We need to learn more about how to prevent and treat this risk.
Q: Will this statement guide physicians toward different treatment protocols?
A: It suggests more of a case-by-case approach in the future as we define these AF thresholds. If studies continue to show worse prognoses with more persistent forms of AF, greater therapeutic aggressiveness to reduce AF burden with drugs, cardioversion or ablation may be beneficial. At the other end of the spectrum, if there is a weak correlation between low AF burden and stroke risk, for example, evidence-supported lifestyle changes might be given priority in the treatment plan. As examples of the latter, weight loss, exercise and even yoga for stress reduction show promise.
Advertisement
More broadly, the evidence we reviewed for this statement underscored the overlap among various cardiovascular epidemics and their shared risk factors, such as obesity, diabetes, tobacco use, hypertension and COPD. This should anchor us more firmly than ever in the need to work with patients, as early as we can, on prevention. Any time we examine a single cardiovascular disease at this level of scrutiny, we are reminded of just how intertwined the morbidities are.
Advertisement
Advertisement
A new CME opportunity in Chicago, May 15-16
After four decades, refinements to the gold standard of bypass continue as new insights emerge
Why definitive surgical closure is the gold standard, and new ways to make it possible
Modified-Bentall single-patch Konno enlargement (BeSPoKE) optimizes hemodynamics, facilitates future TAVR
Cleveland Clinic’s new dedicated program offers nuanced care for a newly recognized cardiovascular risk factor
Scenarios where experience-based management nuance can matter most
Introducing Krishna Aragam, MD, head of new integrated clinical and research programs in cardiovascular genomics
How Cleveland Clinic is using and testing TMVR systems and approaches