Latest research reinforces other recent findings showing minimal risk
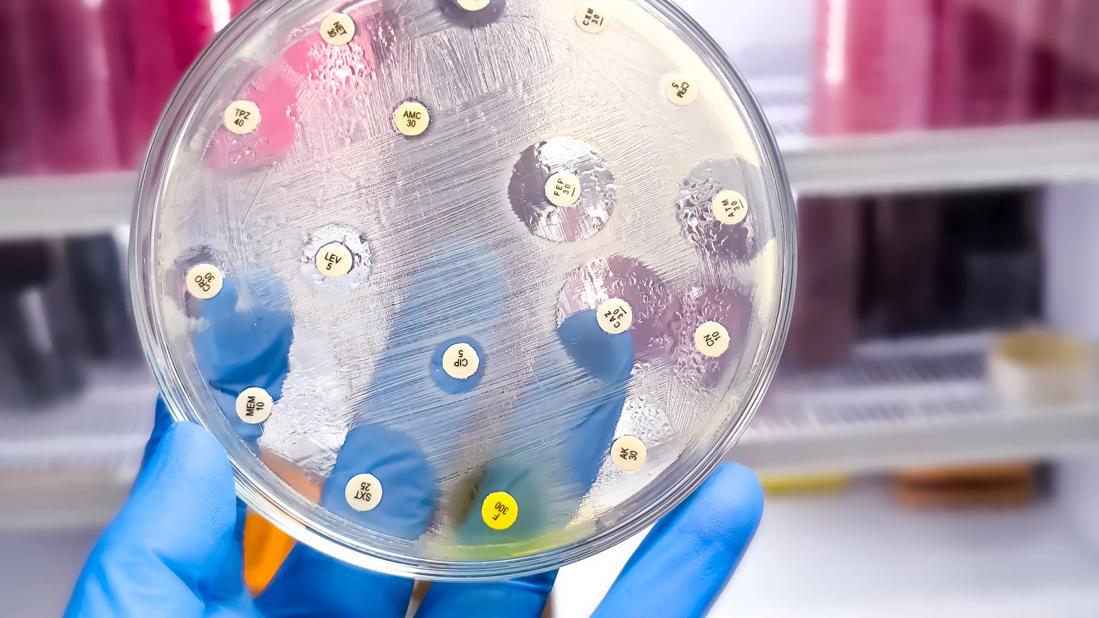
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/34135a98-d532-4549-9609-6f89316db4ff/antibiotic-susceptibility-test-2157592829)
Lab test
A large new multi-institution study led by Cleveland Clinic researchers adds to the body of evidence supporting the safety of biologics use prior to surgery for inflammatory bowel disease (IBD). The research demonstrates that biologic exposure within 60 days of surgery is not associated with postoperative infectious, surgical site infections or anastomotic leaks.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cleveland Clinic colorectal surgeon and Inflammatory Bowel Disease Surgery Section Chief Stefan Holubar, MD, MS, recently presented the team’s findings at the American Society of Colon and Rectal Surgeons’ 2022 annual meeting. The study received the Michigan Society of Colon and Rectal Surgeons Abstract of the Year award at the conference.
In the 23 years since the introduction of the first biologic — infliximab, a tumor necrosis factor alpha inhibitor — to treat Crohn’s disease (CD), and subsequently ulcerative colitis (UC), some research has suggested this class of medication may be associated with increased risk of infections and other postoperative complications in patients who have undergone IBD surgery.
The body of evidence has been inconsistent, with some studies showing a weak association between preoperative biologic exposure and postsurgical complications (usually in patients with CD rather than UC), and others finding no linkage. That variability led many experts to conclude that biologic exposure was a surrogate marker for disease severity rather than an independent predictor of postoperative complications. The issue of whether or when to discontinue preoperative biologic administration was left to individual surgeons to decide.
The availability of large IBD patient datasets and corresponding “big data” analytical capabilities has provided new opportunities to address the question of biologics’ influence on postoperative outcomes.
The Cleveland Clinic-led retrospective review utilized anonymized data from adult patients who underwent IBD surgery between 2017 and 2020 at one of 14 institutions participating in the American College of Surgeons National Surgical Quality Improvement Program IBD (NSQIP-IBD) Collaborative. The NSQIP-IBD, led by Samuel Eisenstein, MD, Director of IBD Surgery at the UC San Diego Health System, collects disease-specific variables relevant to surgical outcomes in IBD to facilitate high-quality, large case-volume research.
Advertisement
The study’s primary outcome measure was any infectious complication, defined as any anastomotic leak, surgical site infection, urinary tract infection, pneumonia, sepsis or septic shock. Secondary outcomes included any surgical site infection or leak. Other outcomes analyzed included postoperative length of stay, readmission, reoperation and overall complications. The primary predictor was exposure to biologics within the 60-day period prior to surgery.
Dr. Holubar and colleagues used propensity score estimated probability of biologic exposure and propensity score weighted conditional logistic regression models to assess the association between patients’ biologic exposure and postsurgical outcomes. They also created backward stepwise multivariable regression models.
Of the 4,578 patients included in the study, 2,282 (50%) were exposed to biologics before surgery and 2,296 (50%) were not. Data showed that patients in the biologics group were more likely to have a CD diagnosis, more comorbidities, and preoperative exposure to steroids and immunomodulators, as well as lower body mass index and albumin levels than their nonbiologic counterparts. Additionally, this cohort was more likely to undergo nonelective surgery, have a colectomy (versus proctectomy or small bowel procedure), and retain a prior ileostomy or have a new one.
None of the analytic methods that Dr. Holubar and colleagues employed identified any association between patients’ preoperative biologic exposure and postoperative infectious complications, surgical site infections or anastomotic leaks (p>0.05 for all models). An exploratory subgroup analysis of patients exposed to biologics and who underwent ileal pouch-anal anastomosis found no association between biologic exposure and anastomotic leaks (p=0.17).
Advertisement
This is the largest nationally representative retrospective cohort analysis to date of biologics’ impact on IBD postoperative outcomes, according to Dr. Holubar. The results “suggest that these agents do not need to be held preoperatively,” he says.
Additionally, preoperative biologic exposure alone shouldn’t preclude anastomotic construction or require a diverting loop ileostomy, Dr. Holubar and his colleagues conclude. Instead, those decisions should be based on whether patients have other known risk factors such as emergency surgery, preoperative infectious complications of IBD, malnutrition or chronic preoperative corticosteroid exposure.
The study’s findings are consistent with results from two other recently published analyses of biologics and postoperative infections using large patient cohorts. Both the Spanish Geteccu Collaborative and the PUCCINI (Prospective Cohort of Ulcerative Colitis and Crohn’s Disease Patients Undergoing Surgery to Identify Risk Factors for Post-Operative Infection I) study concluded that preoperative biologic exposure does not appear to be independently associated with postoperative infectious complications in the IBD patient population.
PUCCINI, led by Benjamin Cohen, MD, Co-Section Head and Clinical Director for Inflammatory Bowel Diseases in Cleveland Clinic’s Digestive Disease & Surgery Institute, was a prospective trial that included 947 patients.
“PUCCINI and our study are very complementary and both confirm the apparent safety of biologics for these patients,” Dr. Holubar says. “They are likely to be the highest quality data we get on this topic because it is very improbable that anyone will conduct a randomized trial” due to funding constraints and other limitations. “Taken together, the findings from these trials demonstrate the safety of biologics and suggest that they do not need to be withheld prior to surgery.”
Advertisement
Dr. Holubar notes that there are other factors to consider before utilizing biologics preoperatively. “While there doesn’t appear to be a reason to hold these agents preoperatively over surgeon concern or fear of an increased infectious complication rate, there is a practical reason to do so,” he explains. “It’s simply a waste of resources to infuse an expensive medication when the target organ is about to be removed.”
Conversely, in CD patients who typically need ongoing biologic therapy, excessive preoperative pausing of the drug may inadvertently cause anti-drug antibodies to develop, leading to secondary loss of response and the need for an alternative agent.
While the research alleviates safety concerns associated with the preoperative use of currently available biologics, Dr. Holubar notes that further study will be required as new drugs are introduced. However, the ability to rapidly collect data remains a challenge.
In addition to the NSQIP-IBD Collaborative, Dr. Holubar and colleagues are working with the Crohn’s and Colitis Foundation’s IBD Plexus program to develop a national collaborative which extends beyond NSQIP data and will also collect data extracted from the electronic medical record, patient-reported outcomes, granular surgeon-entered data regarding variations in surgical technique, and biosamples including serum, tissue and stool. The researchers hope these additional datasets will help address unanswered questions sooner and more efficiently.
Advertisement
Advertisement
Benefits of neoadjuvant immunotherapy reflect emerging standard of care
Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence
Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors
Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling
Potentially cost-effective addition to standard GERD management in post-transplant patients
Findings could help clinicians make more informed decisions about medication recommendations
Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care
Retrospective analysis looks at data from more than 5000 patients across 40 years