A faster, noninvasive way to detect disease
Gastrointestinal graft-versus-host disease (GI GVHD) in patients who have undergone allogeneic hematopoietic cell transplantation (HCT) may someday be diagnosed using a fast, noninvasive test, reports a study conducted at Cleveland Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
GI GVHD is a common complication of HCT, affecting 30-60% of HCT patients, and a significant cause of morbidity and mortality. Currently, it is diagnosed by clinical examination confirmed by endoscopy with biopsy, an invasive, time-consuming procedure that “can be challenging in patients with low blood counts,” says Betty K. Hamilton, MD, of the Blood and Marrow Transplant Program at the Department of Hematology and Medical Oncology at Cleveland Clinic.
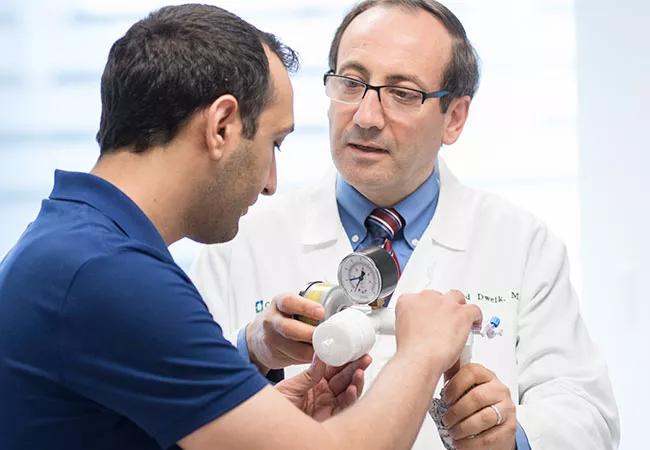
With a need to quickly identify high-risk disease, Dr. Hamilton and colleagues considered another diagnostic method: identification of volatile organic compounds (VOCs) using breath analysis. This technique has shown high accuracy in detecting inflammatory bowel disease (IBD) and efficacy in diagnosing other diseases, such as end-stage renal disease and lung cancer. Raed Dweik, MD, Chairman of Cleveland Clinic’s Respiratory Institute, has spearheaded research on VOCs as a biomarker for 20 years. “The advantage of breath testing is that it is non-invasive and non-intrusive. It does not have a dose limitation like x-rays, an amount limitation like blood tests, or a timing limitation like urine tests. So breath testing can be performed repeatedly as needed,” says Dr. Dweik.
Data have demonstrated an important role of the intestinal microbiome in GI GVHD, with changes in patients who develop GVHD compared to those who do not. It is known that microorganisms can produce volatile metabolites, and thus it is hypothesized that abnormalities in the activity and composition of the intestinal microbiota in disease states may alter the organic compounds produced and expelled in breath.
Advertisement
The study, published in Blood Advances, compared VOCs in 29 patients with and without GI GVHD at day 100 following HCT and 10 healthy controls. The 19 GI GVHD patients had clinically significant GVHD (grade 2-4), with persistent nausea/vomiting or anorexia and/or at least 1 L of diarrhea per day. Using the breath analysis test for VOCs developed by Dr. Dweik’s laboratory, the patients’ exhaled breath samples were analyzed for 22 VOCs using canonical discriminant analysis (CDA). VOCs were analyzed using a logarithmic (log) transformation of each VOC to account for outliers.
The CDA identified five VOCs that differentiated between patients with and without GI GVHD: 2-propanol, acetaldehyde, dimethyl sulfide, isoprene and 1-decene. The model correctly classified 89% and 90% of patients with and without GI GVHD, respectively. Researchers also assessed the correlation between VOCs and GVHD severity. No VOC concentrations were found to have a significant association with GVHD grade.
The study also analyzed the association of VOCs with day 28 response. Of 19 patients, 10 patients achieved complete response (CR), three patients had a partial response (PR), and six had no response. Two VOCs (pentane and ammonia) distinguished patients with CR and less than CR. This model correctly classified 90% of patients with CR and 78% of patients with less than CR. One VOC (acetone) distinguished patients with any response and no response. Patients with higher levels of acetone were less likely to have a response.
Advertisement
A limitation of the study is that half of the GI GVHD patients were exposed to broad-spectrum antibiotics at the time of breath sampling. The 10 patients without GI GVHD did not have an indication for broad-spectrum antibiotics at the time of sampling, although half had recent exposure within the 100-day time period.
“Although a small pilot study, it demonstrated that breath analysis in a transplant and GI GVHD population is feasible and identified a possible “breath signature” that can distinguish GI GVHD and no GVHD. This method may also be able to distinguish between those who had a response to first-line therapy and those who did not. It is exciting that breath analysis could be a possible standard diagnostic method that could replace an invasive procedure in an already sick population,” says Dr. Hamilton.
“Breath analysis for GI GVHD needs a bit more research to confirm the findings and to standardize sample collections and testing. Also, the current equipment is primarily used in a research setting and more work needs to be done to get it to the clinic,” says Dr. Dweik.
The researchers have begun a larger follow-up study that is collecting breath samples from patients before transplant and at day 30 and day 100 following transplant. The samples will be compared with the microbiome. “The hypothesis is that breath analysis and VOCs correlate with the microbiome; thus there can be many implications in following diseases, such as GVHD and even the primary malignancy, throughout the transplant,” says Dr. Hamilton.
Advertisement
Advertisement

Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development

Recent breakthroughs have brought attention to a previously overlooked condition

A review of treatment options for patients who may not qualify for surgery

Looking at the real-world impact and the future pipeline of targeted therapies

The progressive training program aims to help clinicians improve patient care

New breakthroughs are shaping the future of COPD management and offering hope for challenging cases

Exploring the impact of chronic cough from daily life to innovative medical solutions

How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program