A review of conservative, pressure-based and surgical treatments for OSA

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/494d262e-2aac-4786-9b70-dc007813af7a/NEU_4901959_06-19-24_016_LDJ)
CPAP mask
Written by Loufti S. Aboussouan, MD; Aparna Bhat, MD; Todd Coy, DMD and Alan Kominsky, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Note: This article is a slightly abridged version of a review first published in the Cleveland Clinic Journal of Medicine (2023;90:755-765). References have been omitted in this version but are available in the full-length, open-access version available here.
Continuous positive airway pressure (CPAP) remains the gold standard treatment for obstructive sleep apnea, but it is not the only one. Alternative treatments may be better suited to some patients, as this is a heterogeneous disorder with distinct clinical, polysomnographic and physiologic phenotypes.
Here, we review conservative, pressure-based and surgical treatments for obstructive sleep apnea, including their indications, effectiveness, caveats and the patients for whom they might be most effective.
The American Academy of Sleep Medicine bases the diagnosis of obstructive sleep apnea on the apnea-hypopnea index (AHI), i.e., the number of obstructive respiratory events (apnea, hypopnea or respiratory effort-related arousal) per hour of sleep, defined as one of the following:
The Wisconsin Sleep Cohort Study reported that in the years 2007 to 2010, 26% of people aged 30 to 70 had an AHI of at least five and about 10% had an AHI of at least 15 (representing moderate or severe obstructive sleep apnea) and that these were “substantial” increases compared with estimates from 1988 to 1994.
Advertisement
Untreated, obstructive sleep apnea causes daytime sleepiness in more than half of patients and increases the risk of motor vehicular accidents by 17%. Long-term consequences include hypertension, incident diabetes, cardiovascular events and impairment in several domains of cognition, including attention, memory and executive function. Fortunately, the risks of these complications are modifiable with therapy.
Therapy usually includes weight loss, exercise, positional therapy, and alcohol avoidance as adjuncts to CPAP, while other conservative treatments can be alternatives to it (Table 1).
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0e072822-b291-497a-9bd8-a6b8f0a6ecf7/obstructive-sleep-apnea-table-1)
Table 1
The body mass index is an important predictor of obstructive sleep apnea and figures prominently in prediction scales. Conversely, in a longitudinal study, a 10% weight loss predicted a 26% decrease in AHI. Weight loss decreases the collapsibility of the airway as measured by the pharyngeal critical closing pressure, with near-complete resolution of apnea when the pharyngeal critical closing pressure drops below –4 cm H2O.
Lifestyle modifications. In a large long-term randomized study in patients with obesity, diabetes, and sleep apnea, the rate of remission of obstructive sleep apnea at 10 years was 34.4% with intensive lifestyle interventions compared with 22.2% with diabetes support and education only. The improvement in severity of obstructive sleep apnea was related to the change in body weight and to the original AHI.
Bariatric surgery. This approach can significantly improve obstructive sleep apnea, with rates of cure reported as 86%, 57%, and 45%. However, in one study, moderate or severe obstructive sleep apnea persisted in 20% of patients after surgery. In a randomized trial, the reduction in AHI was not statistically significantly greater with gastric banding than with conventional weight loss, even though patients who underwent gastric banding lost more weight. Patients therefore need to be aware that bariatric surgery may not cure their obstructive sleep apnea, and this should be discussed before surgery.
Advertisement
CPAP adherence was poor after bariatric surgery in another study, with patients using their machines on a median of only 49% of nights.
Glucagon-like peptide 1 receptor agonists. These medications can curb appetite and hunger, reduce food release from the stomach, promote postprandial fullness, and have been highly effective in promoting weight loss. They also decrease the AHI by six episodes per hour more than with placebo in one study. Two drugs in this class, liraglutide and semaglutide, are approved by the US Food and Drug Administration (FDA) for chronic weight management. However, no drugs are approved specifically for treating obstructive sleep apnea.
Exercise. Whether exercise alone improves sleep apnea is uncertain. In the Look AHEAD (Action for Health in Diabetes) study of lifestyle interventions including exercise in patients with obesity and diabetes mellitus, the AHI decreased independently of weight change. Similarly, in a meta-analysis, exercise was found to improve obstructive sleep apnea despite minimal weight change. In contrast, in another study in overweight adults with diabetes and sleep apnea, fitness did not change the obstructive sleep apnea severity after accounting for the weight change.
Even so, we recommend exercise for patients with obstructive sleep apnea because it can favorably modify the associated cardiovascular risks.
Positional sleep therapy. The AHI has been observed to be twice as high when people sleep on their back than when they sleep on their side. The increase in AHI in the recumbent position was most prominent in people with less obesity and near-normal weight, and patients with positional sleep apnea tended to have a lower body mass index and lower overall AHI than those with nonpositional sleep apnea.
Advertisement
Positional therapy uses a variety of devices or garments to keep patients off of their back at night, such as pajama tops with a lump or a tennis ball sewn into the back. A Cochrane review found no difference in the Epworth Sleepiness Scale score, quality of life, or sleep quality with positional therapy compared with CPAP. There were 6.4 fewer events per hour with CPAP, but adherence was 2.5 hours longer per night with positional therapy. Compared with scores in a control group, positional therapy improved the Epworth Sleepiness Scale score by 1.58 points (a difference that is not, however, considered clinically important), and reduced sleep apnea by 7.4 events per hour, but 10% of patients still had sleep disturbances and back or chest discomfort.
Alcohol avoidance. In meta-analyses, the prevalence of obstructive sleep apnea was 25% higher in people who consumed alcohol, the duration of apnea was longer, and the nadir oxygen saturation was lower. These effects may be mediated by a selective adverse effect of alcohol on airway dilator muscles, with depression of hypoglossal nerve or genioglossus muscle activity and without changes in breathing pattern, minute ventilation or hypercapnic ventilatory response.
The effect of alcohol on obstructive sleep apnea appears to be particularly pronounced in those with existing snoring or sleep apnea and in men, perhaps reflecting a potential protective effect of progesterone.
No approved pharmacologic therapy
No drug is currently approved or in common use for managing obstructive sleep apnea, and a Cochrane review from 2013 found insufficient evidence to recommend any drug for it.
Advertisement
That said, the antidepressants protriptyline and fluoxetine were both found to reduce the number of events of apnea and hypopnea, in part from their expected effects of reducing rapid eye movement (REM) sleep, but also from a reduction in non-REM events. However, the response was variable, and the drugs did not decrease the number of arousal or desaturation events.
Carbonic anhydrase inhibitors such as acetazolamide, zonisamide and topiramate can reduce the AHI (by 42% in a study of acetazolamide) and improve sleep efficiency and oxygen saturation but not sleepiness. The mechanism may relate to breathing stimulation and reduced ventilatory control sensitivity rather than to improvements in airway collapsibility. For instance, the reduction in the AHI correlates with the reduction in bicarbonate concentration and with reduction in loop gain (i.e., improving an exaggerated ventilatory response upon resumption of breathing following an obstructive event). The AHI is particularly reduced when carbonic anhydrase inhibitors are combined with CPAP. A European Respiratory Society guideline has a conditional recommendation based on low-quality evidence to use carbonic anhydrase inhibitors, but only in the context of a randomized control trial.
A newer strategy is to counteract two mechanisms of pharyngeal hypotonia, namely loss of noradrenergic drive and active muscarinic inhibition, using a combination of noradrenergic and antimuscarinic agents such as atomoxetine with oxybutynin, reboxetine with oxybutynin or atomoxetine with fesoterodine. While neither type of agent alone reduced the AHI, the combination can result in a greater than 50% short-term reduction in the AHI, though the success may depend on targeting patients with a phenotype of milder upper airway collapsibility. These combinations may be promising but are not currently available.
Oxygen
Although oxygen is sometimes empirically prescribed as an alternative in patients unable or unwilling to use CPAP, its use for that purpose is not substantiated. In a meta-analysis of randomized controlled trials comparing CPAP and nocturnal oxygen, both interventions similarly improved nocturnal oxygen desaturation, but oxygen therapy prolonged the duration of sleep-disordered breathing events, may have promoted hypercapnia, and did not improve sleepiness. Further, in patients with obstructive sleep apnea and cardiovascular disease or risk factors for it, oxygen supplementation did not reduce blood pressure, whereas CPAP did.
These findings do not preclude the use of oxygen in patients who have specific endophenotypic traits of sleep apnea. For instance, a multivariable model identified the combination of increased loop gain plus decreased collapsibility or increased pharyngeal compensation as a predictor of a decrease in AHI with oxygen supplementation.
Oral appliances
Oral appliances can be an effective alternative for many patients with obstructive sleep apnea. These devices stabilize and advance the mandible anteriorly to open the airway, especially laterally in the velopharyngeal area. An oral appliance can be a first-line therapy for mild to moderate obstructive sleep apnea and for severe obstructive sleep apnea when a patient cannot tolerate or refuses CPAP.
When obstructive sleep apnea has been confirmed, the patient should be evaluated by a qualified dentist to determine candidacy for an oral appliance based on the health of dentition and existing dental work, relationship of the maxilla to the mandible, mandibular range of motion and history of temporomandibular disorders. The custom-fitted device places the mandible at a comfortable starting position as determined by the dentist and patient, and the device can then be calibrated based on subjective and objective responses within a range comfortable to the patient. When a patient achieves resolution of apnea symptoms, the referring clinician is notified and can confirm treatment efficacy.
Treatment success with oral appliances can be measured in several ways, but often by a decrease in AHI of at least 50%. Using this metric, oral appliance therapy was effective in 68% of 172 patients after two years of treatment in one study. In another study, the success rate was 69%, with success defined as at least a 50% reduction in AHI, coupled with an AHI of 10 or less.
Multiple studies have shown that oral appliances can alleviate daytime sleepiness and mental fog, lower high blood pressure and reduce the risk of cardiovascular-related deaths.
Patients should be seen by a qualified dentist every six months for the first year of oral appliance therapy and then annually. Follow-up is essential to monitor patients for any changes in sleep as well as any device-related side effects such as changes in occlusion or tooth position, jaw pain, temporomandibular joint disorders and damage to existing dental work.
Myofunctional therapy
Myofunctional therapy consists of interventions such as electrical stimulation of the tongue, speech therapy, circular breathing, singing or wind-instrument playing, which strengthen the facial, tongue, oropharyngeal, or skeletal structures and enhance the neuromuscular compensatory mechanisms that counteract the anatomic mechanical loads contributing to airway narrowing. A European task force did not recommend myofunctional therapy as a standard treatment of obstructive sleep apnea, based on limited and low-quality evidence. However, it may have a role for patients seeking alternatives to more effective surgical or mechanical options.
In a systematic review, myofunctional therapy decreased the AHI by 50%, with improvement in oxygen saturation nadir, snoring, and daytime sleepiness. One available electrical tongue-stimulation device (eXciteOSA) is FDA-approved for snoring and mild sleep apnea, and objectively improves snoring, sleepiness, sleep-related quality of life, and AHI (from 10.2 to 6.8 events per hour).
An additional role for myofunctional therapy may be as an adjunct to CPAP to improve CPAP adherence, with potential incremental benefits compared with CPAP alone.
Several types of machines prevent obstructive events by keeping the airway open (Table 2).
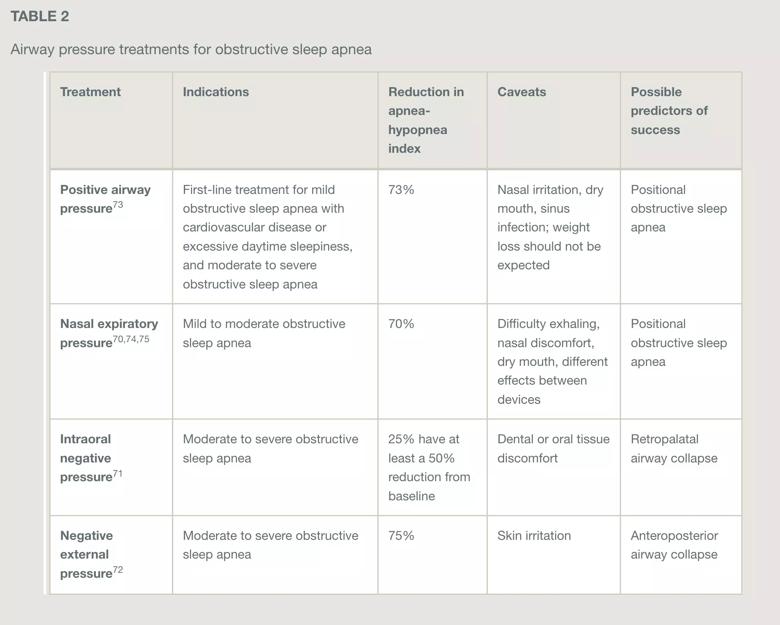
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/73f8cdbe-86a8-42a3-8214-6a50b4e5f21b/obstructive-sleep-apnea-table-2)
Table 2
CPAP is a first-line therapy for moderate or severe obstructive sleep apnea and for mild obstructive sleep apnea associated with comorbidities or cardiovascular risk factors. CPAP machines apply a positive pressure column of air to stent the upper airway and reduce the AHI, often to normal.
CPAP is considered standard of care based on its effectiveness in improving blood pressure control, sleep-related quality of life, and daytime sleepiness, though its effects on cardiovascular risk and glycemic control are less well established. Blood pressure is lowered even in patients with resistant hypertension. There is conflicting evidence on the impact of CPAP therapy on cognition, with some studies demonstrating a signal toward a mild and transient improvement in executive and frontal lobe cognitive function solely in patients with severe obstructive sleep apnea.
In mild symptomatic obstructive sleep apnea, CPAP is recommended if the patient has daytime sleepiness, in which case CPAP can improve quality of life. In a patient with asymptomatic mild obstructive sleep apnea, the decision to use CPAP would be based on a discussion with the patient regarding the potential reduction in cardiovascular risk.
CPAP adherence, particularly in the first few weeks, can be predictive of long-term success with treatment. Insurance companies, including Medicare, require that patients use their CPAP machine for at least four hours on 70% of nights. Ideally, patients should use their device for the entire sleep period. Several factors can be addressed to improve patient comfort and compliance, including the type of mask, expiratory pressure relief, short-term use of hypnotics, cognitive behavioral therapy, and frequent contact with the healthcare team with continued education about the expected benefits. Poor CPAP adherence remains a concern, but adherence at 90 days and even at one year was reported as about 75% in recent studies, which is significantly better than earlier data.
Although CPAP is often touted as facilitating weight loss, there is considerable controversy on this topic, and larger well-conducted studies even suggest that it can cause weight gain as a side effect, owing to a reduced sleep and wake metabolic rates and increased caloric intake.
Automatic or auto-titrating positive airway pressure (APAP) is gaining popularity, as it allows one to prescribe a range of pressures that the device can use to stent the airway based on proprietary algorithms. The pressure range can also be adjusted in the outpatient setting according to compliance reports downloaded from the actual device. Potential benefits of APAP include a lower overall cost with faster initiation of therapy since there is no need for a titration study. Titration studies are therefore becoming less common, though they are still useful to define an APAP pressure range, to meet insurance requirements, or to assist in the appropriate choice of device and pressure settings in more complex cases.
Bilevel positive airway pressure does not have clearly better adherence rates than CPAP but should be considered in patients with sleep-disordered breathing associated with daytime hypercapnia, sleep-related hypoventilation, mixed obstructive and central apnea events, or a high-pressure requirement, or in those who cannot tolerate high expiratory pressures.
Nasal expiratory positive airway pressure devices
Nasal expiratory airway pressure (EPAP) devices are alternatives to CPAP for patients with moderate or mild obstructive sleep apnea. Those devices generate a resistance to expiratory flow and are secured to the nose through nasal inserts with optional headgear (Bongo Rx), or nasal pillows with headgear (OptiPillows, ULTepap). In contrast to CPAP, which provides a continuous pressure through both inspiration and expiration, the back pressure generated by EPAP is present only during expiration with minimal inspiratory resistance. Some of these devices have FDA clearance for mild or moderate sleep apnea (Bongo Rx, ULTepap), and others for snoring only (Optipillows).
In an early study (in 1983), EPAP at 10 cm H2O reduced the number of apnea events, reduced the duration of these events, and improved nocturnal saturation. In currently used devices, the back pressures generated depend on the flow rates, with significant differences in back pressures at similar flow rates between different devices, ranging from one to 14 cm H2O. In a randomized trial of EPAP vs sham therapy, the median AHI was reduced from 15.7 to 4.7 events per hour after one year.
This intervention works across a range of severity of sleep apnea. Ideal candidates may be those with sleep-disordered breathing that has a positional component (worse when supine compared with lateral or prone). However, a randomized trial found no benefit from EPAP in patients with moderate to severe sleep apnea who had discontinued CPAP.
Oral negative pressure therapy
This technique applies negative pressure through an intraoral interface held in place with a flange that fits between the teeth and the lips. The iNAP device is FDA-approved for sleep apnea of any severity. This device improves the retropalatal airway size by displacing the anterior-superior segment of the tongue forward and the soft palate anteriorly and superiorly.
Oral negative pressure therapy may be more effective in sleep apnea with retropalatal collapse than with retroglossal airway collapse, though this was not found in another study. In a review of the intervention, only 25% to 37% of patients had at least a 50% reduction in the AHI and a residual AHI of 10 or less, and a substantial number of patients still had significant obstructive sleep apnea. The baseline severity of sleep apnea did not correlate with success.
Negative external pressure
Continuous negative expiratory pressure is applied by an external silicone collar worn around the anterior neck where it provides negative pressure to open the airway by pulling away the soft tissue structures. As the collar does not cover any facial structures, patients may find it easier to acclimate and adhere to the therapy. The settings of the system are titrated similarly to those of CPAP by increasing the pressure enough to keep the airway open by overcoming the critical airway closing pressure.
In a pilot study, 9 (60%) of 15 patients had an “excellent” response to continuous negative external pressure therapy, defined as reducing the AHI to less than five events per hour (down from a baseline of 43.9.
A newer device can vary the negative external pressure throughout the night and is available in various collar sizes and shapes. In a prospective, open-label trial of this device in 28 patients with moderate obstructive sleep apnea, 14 (50%) had an excellent response and 6 (21%) had a partial response (a decrease in AHI of at least 50% from baseline).
These devices are currently undergoing randomized trials but are not used in practice.
Surgery for obstructive sleep apnea (Table 3) can be considered when a patient has not found success with other therapies. Most sleep surgeons perform drug-induced sleep endoscopy before considering sleep surgery. This procedure is performed with the patient sedated and asleep but spontaneously breathing. Areas of obstruction and collapse can be identified and surgeries to correct these findings can be contemplated.
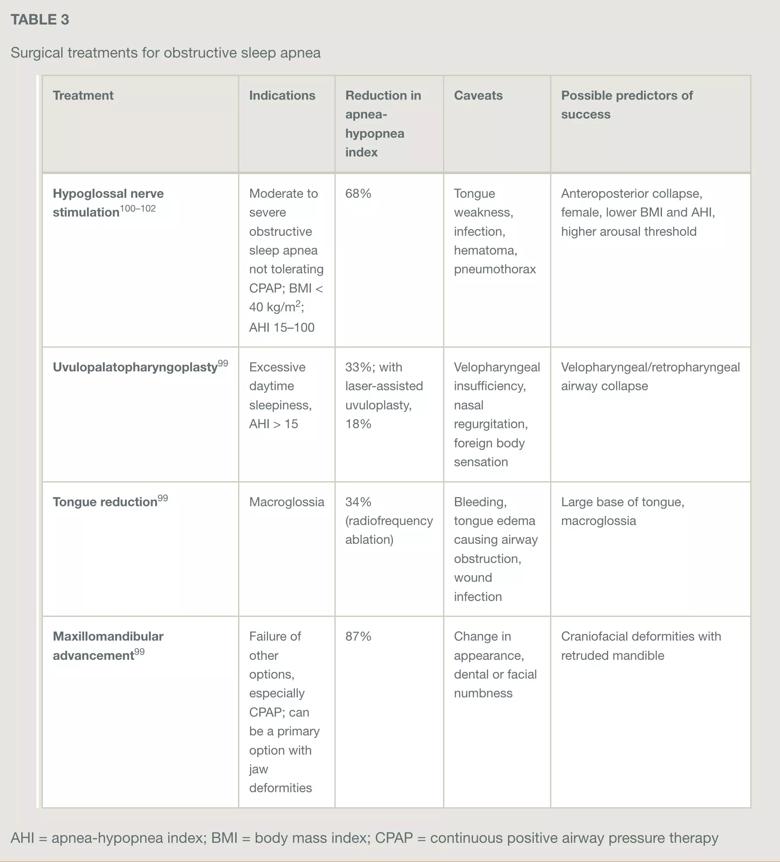
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/226d3886-6b8e-457c-9f07-d2b066a40a54/obstructive-sleep-apnea-table-3)
Table 3
Uvulopalatopharyngoplasty
Surgery for obstructive sleep apnea began in earnest in the early 1980s, when Fujita adapted a procedure used for snoring to treat patients with sleep apnea. Uvulopalatopharyngoplasty has been a mainstay of surgical treatment since that time, with variations and improvements over the years to make it more mucosal-sparing and to address lateral wall collapse.
Success rates vary, as each surgeon uses a slightly different technique. In a meta-analysis based on 15 observational studies (quality of evidence “very low”), the reduction in AHI was 33%. However, over time, the AHI tends to drift back upward because of loosening of scar tissue or change in body weight.
Laser-assisted uvulopalatoplasty, an alternative technique, was found to reduce the AHI by 18% in a meta-analysis of 2 randomized trials (level of evidence “low”).
Tongue reduction
To try to improve the outcomes of uvulopalatopharyngoplasty, surgeons began addressing the tongue. Tongue reduction can be performed in several ways. A midline glossectomy removes an ellipse of tissue in the dorsal surface of the mid-tongue. Radiofrequency treatment can be performed with channeling within the tongue or with needle-tipped prongs to reduce the amount of tongue muscle.
In a meta-analysis of 8 observational studies (level of evidence “very low”), radiofrequency reduction of the tongue was associated with a 34% reduction in the AHI.
Friedman et al created a staging system based on physical findings such as modified Mallampati score (assessment of tongue size and shape vs the oropharngyeal opening) and tonsil size to predict success when performing uvulopalatopharyngoplasty with radiofrequency reduction of the tongue. Patients with a small tongue and large tonsils had the greatest success, while patients with a large tongue and small tonsils had the lowest success rates.
Hypoglossal nerve stimulation
The newest development in sleep surgery has been hypoglossal nerve stimulation. The only commercially available system (Inspire) in the United States was approved by the FDA in 2014 and has been steadily gaining acceptance since publication of the Stimulation Therapy for Apnea Reduction trial. The device consists of an implanted pulse generator, a stimulation lead, and a respiratory sensor lead. The pulse generator augments the neural input of the hypoglossal nerve to the genioglossus and geniohyoid muscles, thereby resulting in protrusion of the tongue forward with each sensed respiration.
Indications approved by the FDA are as follows: adult age 22 or older; candidate must have tried CPAP without success, have an AHI between 15 and 100 events per hour (with no more than 25% of events being central or mixed apneas), and have a body mass index of 40 kg/m2 or less. Also included are patients ages 18 to 21 with an AHI 15 to 100, and pediatric patients with Down syndrome ages 13 to 18 and an AHI 10 to 50 who have not been effectively treated with or who have a contraindication to adenotonsillectomy, and who have failed or cannot tolerate positive airway pressure therapy. Insurance coverage indications may be more restrictive. For a patient to be considered a candidate for hypoglossal nerve stimulation, a drug-induced sleep endoscopy study is required and must show palatal collapse in an anterior-posterior pattern. Concentric collapse is a contraindication. As experience and technology improve, the eligibility criteria will continue to change.
During the implant surgery, three incisions are enough to place the pulse generator and the two leads. The incisions are just below the jaw line and in the upper chest. The procedure is done on an outpatient basis, with the patient under general anesthesia. Once the optimal system settings are obtained through in-laboratory polysomnography, the device is activated by the patient only when going to bed.
Hypoglossal nerve stimulation is associated with high adherence and durable benefits up to five years, consisting of improvements in the Epworth Sleepiness Scale score, patient-reported outcomes comparable with those of CPAP, and reduced AHI.
Initial results showed a 68% reduction in AHI and a 66% success rate (defined as an AHI < 20 and at least a 50% reduction in AHI), but with improved surgical technique and better understanding of device programming, success rates have improved to 75% to 80%. Female sex, lower baseline body mass index, lower initial AHI, and high arousal threshold predict successful therapy.
Studies of cardiovascular outcomes with hypoglossal nerve stimulation are ongoing. Heart rate variability during sleep was noted to improve (decrease), and the improvement correlated with improvement in AHI. In a study at Cleveland Clinic, positive airway pressure therapy lowered diastolic and mean blood pressure more than hypoglossal nerve stimulation. In another study, although diastolic blood pressure declined by 3.7 mm Hg and mean arterial blood pressure declined by 3.7 mm Hg with hypoglossal nerve stimulation, this improvement may be present only in the subset of patients with baseline high blood pressure.
Maxillomandibular advancement
Skeletal surgery can increase the volume of the airway. A combination of a LeFort 1 osteotomy with a bilateral sagittal split of the mandibular rami creates a larger “box” to give more room around the soft tissue contents of the airway. In nine case series in 234 patients, this surgery was associated with an 87% reduction in AHI. However, a study by Kezirian et al found that 30 times more uvulopalatopharyngoplasty surgeries were performed compared with maxillomandibular advancements, suggesting that despite the excellent success rate of maxillomandibular advancement, patients are less accepting of the procedure.
Advertisement
An innovative approach to protecting patients during breast and lung radiation therapy
Screening tool helps flag conditions that warrant further attention
Patients with epilepsy should be screened for sleep issues
A deep dive into the evolution of surgical sleep therapy
Study shows comparable success rates to tongue base dependent epiglottic collapse
Looking at short-term outcomes in a high-risk population
Cleveland Clinic study finds that durable weight loss is key to health benefits
Novel procedures provide options for patients who can’t tolerate CPAP