Real-world study shows high response rates that are durable with commercial lisocabtagene maraleucel
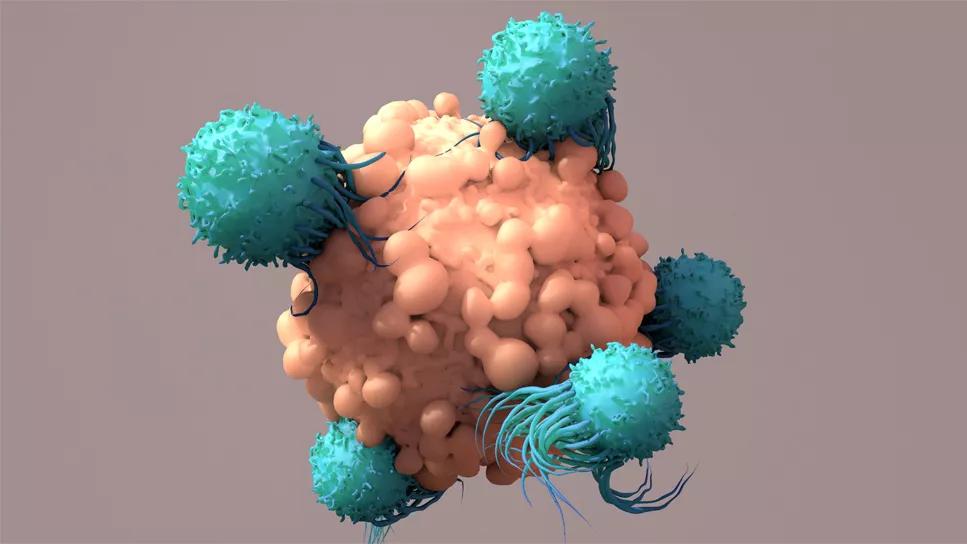
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/20623422-acf7-4841-9d69-0dfb2e5da85f/car-t-cell-richter-transformation-1317697233)
car T-cells
A one-time infusion of lisocabtagene maraleucel (“liso-cel”) led to a high one-year survival rate of 67% with a manageable safety profile in patients with Richter transformation, new research finds.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Up to 10% of patients with chronic lymphocytic leukemia (CLL) develop Richter transformation, in which a newer and more aggressive lymphoma arises. About 90-95% of these are diffuse large B-cell lymphoma (DLBCL). These patients often don’t respond to front-line immunochemotherapy, or progress after initial response. Historically, their median overall survival has been just 3-12 months.
“It’s a very much unmet need,” says Cleveland Clinic hematologist-oncologist Allison Marie Winter, MD, who presented the new study at the annual meeting of the American Society of Clinical Oncology.
However, several newer therapies are offering hope. One is liso-cel (brand name Breyanzi), an autologous, CD19-directed, 4-1BB chimeric antigen receptor (CAR) T-cell product that is approved in the US for treating adults with relapsed/refractory large B-cell lymphoma (LBCL) and CLL/small lymphocytic lymphoma (SLL).
“Liso-cel demonstrated a high overall response rate with deep and durable responses in patients with Richter-transformed DLBCL. The meaningful clinical benefit and expected safety profile in this difficult-to-treat population of patients with Richter transformation is promising,” Dr. Winter says.
The new study is the first of real-world clinical effectiveness and safety of commercial liso-cel in Richter transformation. The data were obtained from the collaborative Center for International Blood and Marrow Transplant Research, of which Cleveland Clinic is a participating center.
A total of 30 patients with Richter transformation who received a single liso-cel infusion between February 5, 2021 and February 5, 2023 were analyzed. The median time from CLL diagnosis to Richter transformation was 49 months, and the time from Richter transformation to liso-cel infusion was11 months. Two patients (7%) had active central nervous system involvement. All but three (90%) had DLBCL histology.
Advertisement
A majority of the patients (23/77%) had received treatment for their CLL prior to their Richter transformations, and all 30 had received treatment for the Richter transformation prior to the liso-cel infusion.
“These patients are clearly high risk. Most had received treatment for their CLL prior to the Richter’s transformation and 37% were dual class exposed to both BTK inhibitors and BCL2 inhibitors. We know that even within CLL, if you’re dual-exposed, it’s a high-risk situation,” Winter notes.
During a median follow up of 12.3 months, the overall response rate to liso-cel was 76%, with 66% achieving complete response. The median time to first response was 1.1 months. The median duration of response was not reached, and the 12-month duration of response was 77%. At 12 months, median progression-free survival was 54%, and overall survival 67%. “That's an impressive response rate and durability of response in this high-risk group,” Dr. Winter says.
The safety profile of liso-cel in RT was similar to that typically seen with CAR T-cell therapy.
While 21 of the 30 patients (70%) experienced cytokine release syndrome (CRS), in 18 it was mild (grade 1 or 2). Fourteen patients (47%) experienced immune effector cell-associated neurotoxicity syndrome (ICANS), and of those, eight were grades 3 or 4. Treatment for CRS and ICANS was successful for most patients.
“When we think about CAR T-cell safety, we're always looking at CRS and ICANS. Here, nearly a third did not experience CRS, and over half didn’t develop ICANS. The low incidences of grade ≥ 3 CRS and ICANS demonstrates the favorable safety profile,” Winter says.
Advertisement
Other adverse events included hypogammaglobulinemia in 22 (73%), clinically significant infection in 13 (43%) and prolonged cytopenias in five (17%). Eight patients died, seven due to primary disease progression and one due to CRS. (That patient also had hemophagocytic lymphohistiocytosis.)
Cleveland Clinic providers specialize in both CLL and CAR T-cell therapies, and have conducted numerous studies in this area. Dr. Winter notes that for research into liso-cel in Richter’s transformation, longer follow-up in a larger cohort is needed to understand the full benefit of liso-cel in this patient population.
Advertisement
Advertisement
Age alone should not rule out patients from potentially curative treatment
Higher type 2 immunity observed in persistent CAR T cells
Minimal residual disease testing shows promising results
Dispelling myths and sharing practical experiences
Addressing rare disease and challenging treatment course in an active young patient
Early results show patients experiencing deep and complete response
The latest evidence to support ‘practice-changing’ protocol—and a note of caution
Study measures real-world outcomes for relapsed or refractory large B-cell lymphoma