Optimized responses in transplant- and CAR T-cell therapy-eligible patients
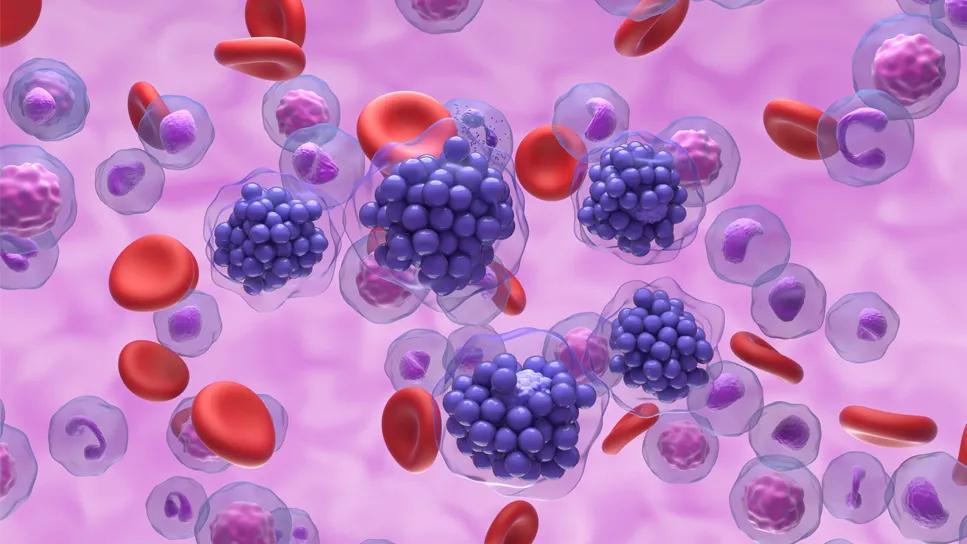
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2744372a-5d4a-4c7e-89ff-2027a430fff0/favorable-efficacy-large-b-cell-lymphoma-2154408799)
Diffuse large B-cell lymphoma
Patients with relapsed or refractory (R/R) diffuse large B-cell lymphoma (DLBCL) have benefited from recent advances in immunotherapies such as chimeric antigen receptor T-cell therapy (CAR-T). CD3/CD20-directed bispecific antibodies like glofitamab have recently received FDA-approval, and have shown efficacy in the treatment of DLBCL when the disease recurs after two or more treatments. Recent data from a multicenter study demonstrates that combining glofitamab with salvage chemoimmunotherapy is safe and effective for patients with R/R DLBCL who are eligible for autologous stem cell transplant (ASCT) or CAR T-cell therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Standard second-line chemoimmunotherapy will not achieve response in approximately 50% of patients with relapsed DLBCL. The addition of glofitamab to chemoimmunotherapy may provide an optimal bridge to transplant or CAR T-cell therapy by achieving disease control in a larger number of patients,” says Paolo F. Caimi, MD, study co-author and staff oncologist at Cleveland Clinic Cancer Institute.
Dr. Caimi’s previous work has shown that a subgroup of patients with DLBCL who relapse early may still remain chemosensitive, and may benefit from the incorporation of the recent advances in second- and third-line treatments, improving outcomes in patients with DLBCL.
Bispecific antibodies are a novel immunotherapy for patients diagnosed with R/R DLBCL. They act by bringing T-cells in proximity to the malignant B cells, leading to T-cell mediated cytotoxicity. The current phase 1b study, presented at the 2024 American Society of Hematology meeting, was aimed at evaluating the safety and response rates of the combination of glofitamab with chemoimmunotherapy, including rituximab, ifosfamide, carboplatin and etoposide (glofitamab-R-ICE).
Eligible patients were diagnosed with DLBCL or high-grade B-cell lymphoma, had received one prior line of therapy and were considered eligible to receive subsequent treatment with CAR T-cell therapy or ASCT. Investigators measured overall response rate (ORR) by 2014 Lugano criteria, the proportion of patients that achieved complete or partial metabolic response (CMR; PMR) within three cycles of glofitamab-R-ICE. Patients could receive two or three cycles of glofitamab-R-ICE at the investigators’ discretion, with responding patients proceeding to CAR T-cell therapy or ASCT.
Advertisement
Forty-one patients with a median age of 66 years received treatment in the study. Most of the patients were white men (6.59% white, 71.1% men). DLBCL not otherwise specified was the most common histological subtype (70.7%), and 39.0% of patients had extranodal disease. The median treatment duration was 28 days (range: 1 - 65).
Interim analysis showed ORR (CMR or PMR) of 78.1% (95% CI: 60.0 - 90.7) and a CMR rate of 68.8% (95% CI: 50.0 - 83.9) (N = 32). Among the patients who had one or more doses of any study treatment, the most common adverse event (AE) was cytokine release syndrome (CRS), grades 1 and 2, with no grade 3 CRS and no immune effector cell-associated neurotoxicity syndrome (ICANS) events reported. Grade 3 and 4 AEs occurred in 61.0% of patients, and no fatal AEs were reported.
“For our patients who don’t respond to salvage chemoimmunotherapy, this combination is yet another step toward better disease control before transplant or CAR T-cell therapy,” says Dr. Caimi. “These are very encouraging, and I hope lead to additional questions, like whether further therapy is needed for some patients and whether CAR T-cell therapy or ASCT is the best consolidation strategy after very effective regimens such as glofitamab-R-ICE. This of course requires further study, in particular with regards to the duration of disease remission.”
With a promising safety profile, low treatment discontinuation rate and high response rates, this combination therapy adds another option to the complex conversation about optimal salvage therapies and sequences for patients with DLBCL, many of whom have disease that is refractory to standard chemoimmunotherapy.
Hear our recent podcast about bispecific antibodies and immunotherapy for treating aggressive lymphomas.
Advertisement
Advertisement
Addressing rare disease and challenging treatment course in an active young patient
Study measures real-world outcomes for relapsed or refractory large B-cell lymphoma
CAR T-cell therapy, bispecifics and antibody drug conjugates have changed disease management
Global R&D efforts expanding first-line and relapse therapy options for patients
Two thirds of patients responded to CAR T-cell therapy
62% of patients were progression-free at 18 months post-transplantation
Distinct molecular features found in five subtypes of disease
Patients who relapse early after first-line chemotherapy are often, but not always, refractory to second-line chemotherapy