During global health crisis, investigational drug proves successful
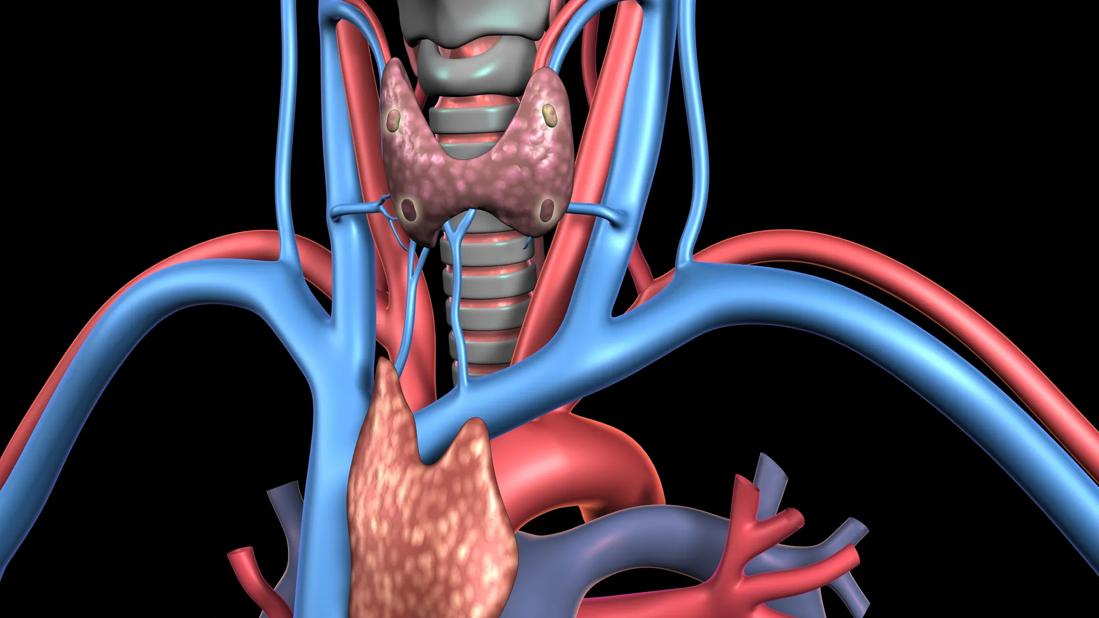
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a9c8268f-a354-4d2f-bc8c-660af6ca5ccb/thyroid-parathyroid-and-thymus-gland-jpg)
Thyroid
When Cleveland Clinic oncologist Jessica Geiger, MD, first began caring for a 46-year-old woman with metastatic papillary thyroid cancer in early 2019, Dr. Geiger prescribed the standard treatment, lenvatinib. But, just as COVID-19 swept across the country, the patient’s cancer began to progress rapidly. She ended up in Cleveland Clinic’s intensive care unit (ICU), leaving both her and Dr. Geiger searching for answers during an already-uncertain time.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Trouble breathing, new pain in her bones, hip and neck, and multiple lesions in her spine — these were all popping up for my patient in early 2020,” Dr. Geiger says. “She had been on lenvatinib, which was proving itself ineffective.”
Lenvatinib, a multikinase inhibitor, is a targeted therapy that doesn’t require cancer-specific mutations. However, because lenvatinib has several targets within the signaling cascade, there are many resulting side effects.
“Side effects — flu-like symptoms, high blood pressure, loss of appetite, overwhelming fatigue — were coming from the medication, not just the cancer itself,” Dr. Geiger says. “Patients accept a great deal of toxicity when the goal is to cure the cancer. But in this case, we’re trying to control the disease knowing we won’t cure it. In that regard, when the goal is to feel better and have a better quality of life, it’s hard to justify treatment.”
On March 18, just as COVID-19 was sweeping across the country, Dr. Geiger’s patient was hospitalized at Cleveland Clinic main campus, then transferred to the ICU. Her symptoms — shortness of breath and a continuous cough — largely mirrored those of COVID-19.
Dr. Geiger and the clinical research team at Cleveland Clinic Cancer Center were able to initiate treatment with investigational drug LOXO-292, now called selpercatinib, while the patient was in the ICU. Selpercatinib (LOXO-292) is a highly selective and potent small molecule RET kinase inhibitor.
“Caregivers in the hospital, ICU nurses and research and clinical coordinators came together to provide incredible patient care, even in the midst of so much fear and anxiety surrounding a global health pandemic,” Dr. Geiger says. “We were on the front line and yet continued to provide excellent bedside care.”
Just two days after initiating selpercatinib (LOXO-292), the patient was transferred out of the ICU. And two days after that, she was discharged from the hospital.
“From being in respiratory failure to going home on minimal oxygen — in a span of just four days — is incredible,” Dr. Geiger says.
Advertisement
The Food and Drug Administration (FDA) approved selpercatinib (LOXO-292) during the summer of 2020.
The selective RET inhibitor selpercatinib is safe and effective in both treated and treatment-naïve patients with RET fusion-positive non-small cell lung cancer (NSCLC), according to the results of a phase 1/2 clinical trial recently published in August 2020 in New England Journal of Medicine. RET fusions have been identified in 1% to 2% of NSCLC cases and have been associated with a high risk of developing brain metastases. Dr. Geiger’s patient’s thyroid cancer, specifically papillary thyroid carcinoma, harbors the RET fusion that selpercatinib targets. These fusions are found in 10-20% of all papillary thyroid carcinomas.
“We have kinase inhibitors that inhibit the RET proto-oncogene,” says Nathan Pennell, MD, PhD, coauthor of the study and Director of Cleveland Clinic Cancer Center’s Lung Cancer Medical Oncology program, “but the clinical benefit from these was modest at best for RET fusion-positive patients. The introduction of selpercatinib three years ago changed the game a bit, and now we have some early results showing promise.”
Promise that Dr. Geiger witnessed firsthand. “Seeing my patient in May was like seeing a new person. She was in a much better place,” Dr. Geiger says. The patient continues to receive selpercatinib and requires two liters of oxygen a day. “During a global health crisis, our team at Cleveland Clinic delivered expert patient-centered care while also keeping each other safe.”
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches