Tumor downsizing and en bloc resection are keys to treatment
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 72-year-old man with gradual narrowing of his stool caliber and increasing need for stool softeners was referred for evaluation to Hermann Kessler, MD, PhD, senior expert in minimally invasive surgery in Cleveland Clinic Digestive Disease & Surgery Institute’s Department of Colorectal Surgery.
The patient had anorexia but reported no weight loss, rectal bleeding or abdominal pain. He had a history of hypercholesterolemia, hypothyroidism and atrial fibrillation. He had no family history of colorectal cancer or inflammatory bowel disease. He had never undergone a colonoscopy.
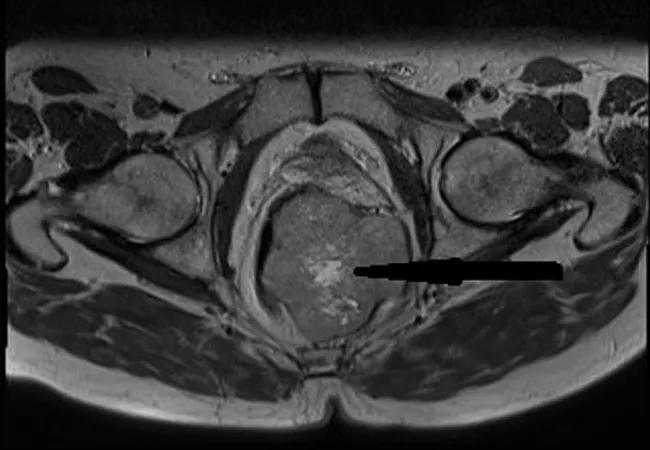
Digital rectal examination revealed a hard mass palpable on the left posterior rectal wall, overlaid with normal mucosa, which was confirmed by colonoscopy. CT and MRI identified an 8 x 5.4 x 7 cm mass originating in the lower rectum and abutting the prostate and internal sphincter muscle. The neoplasm had invaded the muscularis but not the perirectal fat.
CT-guided biopsy and immunohistochemical staining confirmed a rectal gastrointestinal stromal tumor (GIST). There was no evidence of distant metastasis.
The patient was treated with radiation and neoadjuvant imatinib to shrink the tumor prior to undergoing abdominal perineal resection. A vertical rectus abdominis myocutaneus flap was harvested and used to fill the perineal defect.
Eighteen months after surgery, the patient is comfortable with his colostomy and doing well. He will continue to be monitored with periodic CT scans according to National Comprehensive Cancer Network (NCCN) guidelines.
Advertisement
An axial MRI depicts the gastrointestinal stromal tumor originating in the lower rectum. Reproduced from Connelly TM, Clancy C, Hu S, Steele SR, Kessler H. A Low rectal GIST. BMJ Case Rep. 2022 Mar 14;15(3):e248505. Copyright 2022. Used with permission from BMJ Publishing Group Ltd.
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8ad56340-6fe8-4f62-9c0e-c4be18e104f1/22-DDI-2887482-Low-rectal-GIST-gallery-1-800x550-1-150x114_jpg)
Extraction of the transperineal specimen. Reproduced from Connelly TM, Clancy C, Hu S, Steele SR, Kessler H. A Low rectal GIST. BMJ Case Rep. 2022 Mar 14;15(3):e248505. Copyright 2022. Used with permission from BMJ Publishing Group Ltd.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/dd74db24-2dbf-4f83-8bbf-e3f0d4cd5484/22-DDI-2887482-Low-rectal-GIST-gallery-2-800x550-1-150x114_jpg)
Placement of the vertical rectus abdominis myocutaneus flap in the perineal defect. Reproduced from Connelly TM, Clancy C, Hu S, Steele SR, Kessler H. A Low rectal GIST. BMJ Case Rep. 2022 Mar 14;15(3):e248505. Copyright 2022. Used with permission from BMJ Publishing Group Ltd.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/320f10f2-7bfe-45c9-a25a-5fa52af094ab/22-DDI-2887482-Low-rectal-GIST-gallery-3-800x550-1-150x103_jpg)
A low rectal GIST is a rare diagnosis. GISTs comprise only 0.1% to 3.0% of gastrointestinal malignancies, and only 4% to 5% of all GISTs are rectal GISTs.
Consult QD asked Dr. Kessler to describe how he diagnosed this tumor and the surgical approach he used to treat it.
Dr. Kessler: We could palpate the tumor, but when we scoped the patient, we found the mucosa was totally preserved. This ruled out adenocarcinoma of the rectum, which arises from the mucosa. The bulge made a submucosal lesion more likely. A biopsy performed under CT guidance revealed characteristics consistent with GIST.
Dr. Kessler: It was clear that surgical resection would be necessary, but the smaller the tumor is at the time of resection, the better the long-term chance of achieving a cure. This is why it’s always worth trying to downsize and downstage the tumor.
Advertisement
When this patient was discussed in our multidisciplinary tumor board, the oncologists recommended trying radiotherapy and imatinib therapy. After six cycles, the tumor was reduced but remained 6.4 cm in diameter and had invaded the rectal wall.
Dr. Kessler: We performed a laparotomy and en bloc resection with extralevator abdominoperineal resection.
It is clear from previous surgeries that if you don’t take the levator muscle, you may end up with a situation where the lateral resection line is very close to the tumor. This is why rectal tumors removed by abdominoperineal resection in older studies had higher recurrence rates.
Extralevator abdominoperineal excision is a newer technique that ensures the external and internal sphincter are taken appropriately. If the internal sphincter is involved, the external sphincter provides a safety barrier to avoid cutting close to or through the tumor. The approach was developed by Torbjörn Holm [of the Karolinska Institute] in Sweden. I operated with Dr. Holm during my time in Germany and learned first-hand how he proceeded with these cases. This patient was an ideal candidate.
Dr. Kessler: We could have mobilized the rectum laparoscopically. However, the very distal location of the tumor demanded an abdominoperineal excision, so a large perineal excision would have been needed anyway. The perineal defect was covered with a vertical rectus abdominus myocutaneous (VRAM) flap, which required making a large longitudinal incision in the abdomen. It would have made no sense to first mobilize the tumor laparoscopically and then have the plastic surgeon make a large longitudinal incision for the VRAM flap. It was easier, faster and less risky for the patient to do the entire operation through a traditional abdominal midline incision.
Advertisement
Dr. Kessler: NCCN guidelines provide a schedule for monitoring the patient with CT.
Dr. Kessler: They should listen to the patient. If they present with minor symptoms like stool-caliber changes, even in the absence of bleeding, or pain in the lower pelvis, check the rectum. If they see an unfamiliar lesion, or a lesion they are not comfortable with, they should consider referring the patient to an institution such as Cleveland Clinic with rectal specialists.
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years