Addressing rare disease and challenging treatment course in an active young patient
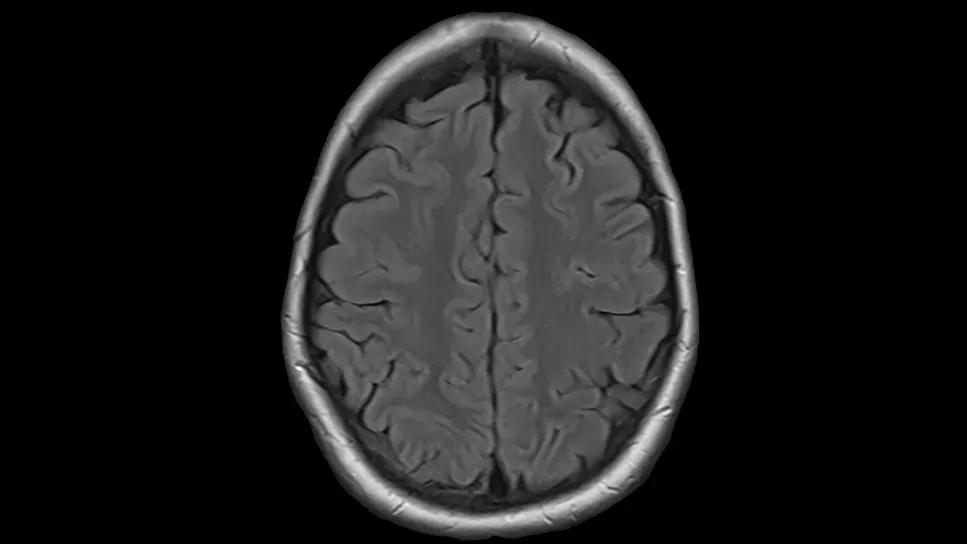
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/82c95798-6980-42f5-8ad3-4781cf553d83/bone-marrow-transplant-in-lymphoma-patient-scan-1)
PET scan
A 21-year-old patient with aggressive lymphoma sought care at Cleveland Clinic Cancer Institute after rapid acceleration of her disease. Caring for a young patient with lymphoma and swift progression to central nervous system (CNS) disease required a thoughtful approach. After stabilizing the patient, the Hematology team at Cleveland Clinic Cancer Institute prepared her for a bone marrow transplant using a newer medication that’s typically used to treat a certain type of lung cancer that shares the same genetic mutation as her disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A female college student was being treated for T-cell lymphoma at a nearby cancer center. Typically, patients with CD30 positive T-cell lymphoma respond to brentuximab vedotin-containing chemotherapy regimens. However, she was refractory within a month of starting this treatment, with new lesions in her brain. She was hospitalized with headaches, nausea and extreme fatigue.
The patient was already scheduled to see the Medical Director of the Inpatient Lymphoma Myeloma Service, Deepa Jagadeesh, MD, in her clinic for a second opinion. Many physicians refer patients with this disease to Dr. Jagadeesh based on her experience of caring for this rare condition. Unfortunately, the patient was hospitalized and needed immediate intervention. Because of this, Cleveland Clinic Cancer Institute quickly facilitated a hospital-to-hospital transfer to start a treatment plan.
As with all T-cell lymphomas, the care team needed to work quickly to prepare the patient for an allogeneic bone marrow transplant. An allogeneic stem cell transplant involves transfusing stem cells from a matched related or unrelated donor. Unfortunately, there wasn’t a full-match donor in the national donor registry. Her sister was a half match, so the team proceeded using her sister’s cells.
Data from studies show that the success rate is comparable when patients receive stem cells from a fully matched or half-matched donor. In cases where there is a half match, patients receive a different conditioning treatment to mitigate the risk of delayed engraftment and graft-versus-host-disease (GVHD).
Advertisement
Treating T-cell lymphoma in the brain required a creative approach. Dr. Jagadeesh decided to put the patient on a newer tyrosine kinase inhibitor that’s approved for patients with lung cancer with an anaplastic lymphoma kinase (ALK) mutation. This drug was used since her lymphoma also had this same genetic mutation. “There are case reports showing this drug delivers a good response in relapsed/refractory T-cell lymphoma patients with the ALK mutation, even with CNS disease,” says Dr. Jagadeesh.
The patient was in college in Michigan when she was first diagnosed. This was a lot to take in, and as with all young people with cancer, it was essential to ensure she had the emotional and psychosocial support to get through the transplant as smoothly as possible. It’s been recognized in the medical community that young patients’ brains work a bit differently, and they may feel particularly isolated from their peers, especially when they’re very sick and must be away from family and friends.
The care team’s goal was to ensure that the patient and her family had emotional and psychological support and resources to get through this process. The Behavioral Health team provided the patient with support for anxiety and depression, which are common in patients facing such a long treatment trajectory. Her nurses, nurse coordinator and social worker were there from the start and throughout her transplant journey.
Her nurse coordinator shared updates with Dr. Jagadeesh in between her visits. “She felt close to her care team, and was comfortable talking about her disease and its impact on the rest of her life,” says Dr. Jagadeesh. Patients undergoing bone marrow transplants also need to stay close to the clinic for the first 100 days after the procedure, and this can be a financial and logistical hurdle. The social worker identified residential options to try and help reduce this burden for her family.
Advertisement
The patient’s social support was very strong. Her parents were with her during her whole hospitalization, staying positive and asking good questions to advocate for her.
During the treatment, she experienced minor GVHD, which resolved after topical treatment, as well as GI issues, which were treated with steroids. The Palliative Care team supported her inpatient as well as after discharge to manage pain.
Now nearly a year out from her bone marrow transplant, the patient is in complete remission. She is not on any maintenance therapy.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2e1d1ed9-71c8-4878-baca-3bdc1dcbfbd4/bone-marrow-transplant-in-lymphoma-patient-scans-inset)
As a next step, she’ll participate in the Survivorship program, which involves undergoing a comprehensive checkup and testing. She’s currently seen for monthly check-ins. If all goes well, she will graduate to quarterly follow-ups with Hematology soon.
She’s living independently and completing her undergraduate degree. Her interactions with social work inspired her to pursue this as a career path. She will begin her graduate program in social work in early 2026. “It’s been a long journey and she’s in a very happy place,” says Dr. Jagadeesh. “I’m so pleased for her.”
There were several key takeaways from this case.
Choosing treatment for rare disease can be challenging. “It can be frustrating when there are limited treatment options available,” says Dr. Jagadeesh. “We’re making some strides and advancements, but treatment for this rare disease remains limited. In this case, since the patient’s disease shared an ALK alteration with a certain type of lung cancer, we were able to leverage that lung cancer treatment for get her disease in remission.”
Advertisement
Understanding the emotional journey of the patient is essential. “There was early discussion of transferring the patient to a pediatrics floor so she could take advantage of their additional support services, but as a mature young adult, we didn’t think she would feel as comfortable there or want to change providers once she had established relationships here,” says Dr. Jagadeesh.
Being diagnosed with cancer is life-altering at any age, but young adults with cancer may have unique concerns. “Young patients have a difficult time when diagnosed with cancer as their lives revolve around college and friends,” says Dr. Jagadeesh. “It can be hard to understand and accept that this is a long journey, especially after relapsing with CNS disease. And it’s tough for any 21-year-old to be in a hospital bed for weeks, losing their hair and not seeing their friends.
Adapting to these changes is very difficult. She overcame these challenges very well. It’s wonderful to see this young person who faced such difficulties come out well and decide to give back to the community.”
Advertisement
Advertisement
Study measures real-world outcomes for relapsed or refractory large B-cell lymphoma
Optimized responses in transplant- and CAR T-cell therapy-eligible patients
CAR T-cell therapy, bispecifics and antibody drug conjugates have changed disease management
Global R&D efforts expanding first-line and relapse therapy options for patients
Two thirds of patients responded to CAR T-cell therapy
62% of patients were progression-free at 18 months post-transplantation
Distinct molecular features found in five subtypes of disease
Patients who relapse early after first-line chemotherapy are often, but not always, refractory to second-line chemotherapy