Distinct molecular features found in five subtypes of disease
Making marked improvements in outcomes of frontline treatment of diffuse large B-cell lymphoma (DLBCL) will require targeted agents based on the molecular features of the disease, according to a new paper published in Expert Review of Hematology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
To date, DLBCL has been treated as a single disease and newly diagnosed patients have been given the same course of treatment of rituximab, cyclophosphamide, hydroxydaunorubicin hydrochloride (doxorubicin hydrochloride), and vincristine (Oncovin). Known as R-CHOP, this course results in sustained remission for roughly 60-70 percent of patients. Relapses are usually correlated with high-risk molecular features, including mutation or deletion of TP53 gene. Despite advances in refractory disease management, such as CAR T-cell therapy, outcomes remain poor for a segment of this population.
Researchers have been working for decades to understand how best to improve front-line treatment. Most efforts to improve those outcomes have been unsuccessful until last year, when randomized phase 3 POLARIX trial data demonstrated that the use of the anti-CD79B antibody drug conjugate POLIVY® showed improvements over R-CHOP.
CD79B is a component of the B-cell receptor expressed in B-cell malignancies such as DLBLCL. POLIVY is the combination of the monoclonal antibody polatuzumab and a targeting agent called vedotin. Polatuzumab attaches to CD79B positive cancer cells and delivers the vedotin to eradicate them.
The POLARIX study enrolled 879 newly diagnosed patients aged 18-80 with International Prognostic Index (IPI) scores of 2-5, and compared R-CHOP to R-CHOP with POLIVY (Pola-R-CHOP). Patients were randomly assigned to receive six cycles of Pola-R-CHOP or R-CHOP, plus two cycles of rituximab alone. The two-year progression-free survival was 76.7% with Pola-R-CHOP vs. 70.2 with R-CHOP. There was no overall survival difference between the two treatment arms, though fewer patients who received Pola-R-CHOP required subsequent treatment.
Advertisement
“There’s a general expectation that Pola-R-CHOP will most likely become the new standard of care for newly diagnosed patients with DLBCL in the near future,” says Brian T. Hill, MD, PhD, Director of the Lymphoma Program and article co-author.
One notable finding of the study highlighted the need to better understand DLBCL subgroups. The two major subgroups of DBLCL are germinal center and activated B-cell, the latter of which typically has poorer outcomes. However, in the POLARIX study, those patients in the activated B-cell subgroup seemed to gain more benefit from Pola-R-CHOP than patients in the germinal center subgroup. “Though the study wasn’t designed to test whether one subgroup of patients had a preferential benefit over another, those findings are very provocative,” says Dr. Hill. “Even within the activated B-cell subtype, we may find there are subgroups that have preferential benefit from polatuzumab vedotin or other targeted agents.”
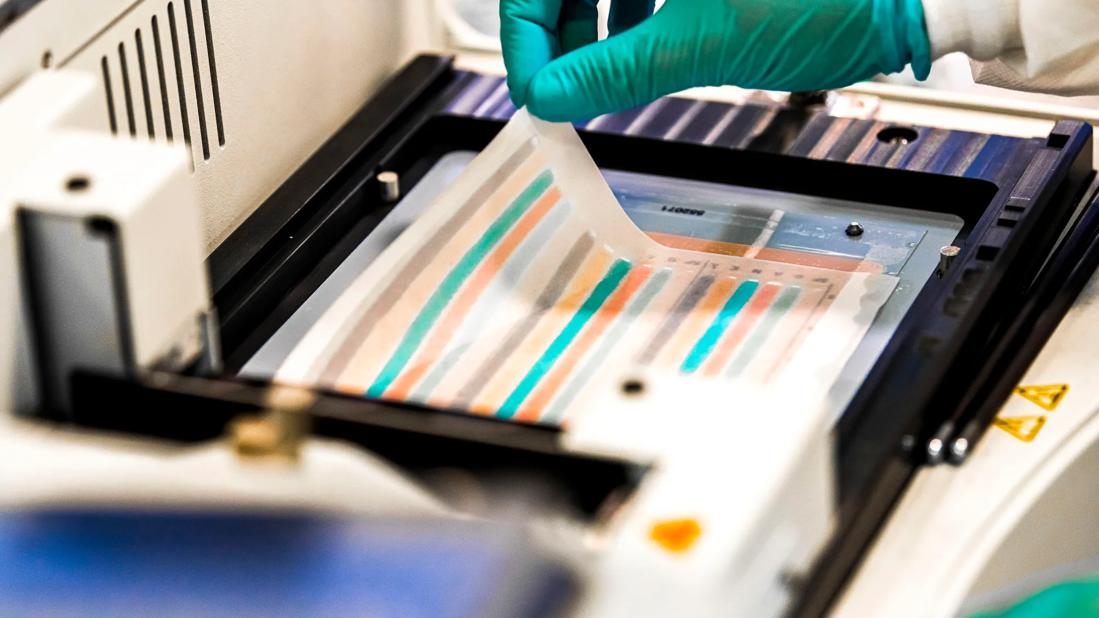
The hope is that researchers can better understand the mutations involved with different subsets of DLBCL in order to develop more targeted agents for treating each type of the disease. “We are also likely going to be embarking on a new era where sophisticated molecular profiling is performed on patients’ tumors to determine their risk profile and identify molecular abnormalities that are potentially targetable by individual medications,” says Dr. Hill.
As a member of the National Cancer Institute’s Eastern Cooperative Oncology Group (ECOG) lymphoma committee, Dr. Hill is leading a research team that is planning to embarking on a “match protocol” whereby patients will be given R-CHOP, R-CHOP with polatuzumab vedotin or an additional targeted agent based on the molecular features of the tumor.
Advertisement
Though there is not yet one reliable, reproducible assay for determining subtype, Dr. Hill says plans are underway to test how well assays will perform in the real-world setting so that they may one day become part of clinical practice. “Historically, by treating all patients the same, it’s been very difficult to move the needle,” says Dr. Hill. “DBLCL has been treated like one disease when in all probability, it is at least four to five different subgroups.”
Until then, clinicians will continue to rely on risk assessment tools such as LDH levels and IPI scores. Hill anticipates in the future there will likely be additional approaches to risk assessment, including real-time monitoring of minimal residual disease in the blood.
As researchers better understand disease subtypes, the goal is to more accurately prescribe the appropriate treatment. For example, roughly 10% of newly diagnosed patients have double-hit DLBCL, which is typically managed with a dose-adjusted R-CHOP or a slightly more intensive chemotherapy regimen of rituximab, etoposide, prednisone, vincristine, cyclophosphamide and doxorubicin (EPOCH). Data suggests that EPOCH improves outcomes, though there has yet to be a head-to-head study of this subgroup of patients.
In the meantime, Dr. Hill recommends that newly diagnosed patients receive FISH testing for translocation of BCL2 and BCL6 to determine if they have double hit-lymphoma. For younger patients who can tolerate more intensive regimens, it may be appropriate to refer them to a tertiary cancer center for therapy such as EPOCH, which requires a five to six-day hospitalization at the start of each three-week cycle.
Advertisement
While the prospect of polatuzumab vedotin for front-line treatment holds promise, the benefits are not subtype specific. Standard molecular assays that integrate multiple genomic approaches are needed, as well as the ability to detect circulating tumor DNA to better understand the mutation profile of each patient’s disease. Having a standard approach to understanding the molecular subtype of DLBCL will allow for trials to test specific pathway inhibitors against each subtype.
Advertisement
Advertisement

Addressing rare disease and challenging treatment course in an active young patient

Study measures real-world outcomes for relapsed or refractory large B-cell lymphoma

Optimized responses in transplant- and CAR T-cell therapy-eligible patients

CAR T-cell therapy, bispecifics and antibody drug conjugates have changed disease management

Global R&D efforts expanding first-line and relapse therapy options for patients

Two thirds of patients responded to CAR T-cell therapy

62% of patients were progression-free at 18 months post-transplantation

Patients who relapse early after first-line chemotherapy are often, but not always, refractory to second-line chemotherapy