A recent case study illustrates surgical intervention for treating recurrent bladder cancer
An otherwise healthy six-year-old boy initially presenting with pain and burning with urination was diagnosed with stage 3 embryonal rhabdomyosarcoma of the bladder. After receiving chemoradiation locally near his home in rural Pennsylvania, he was rendered disease free for nearly two years before the disease relapsed.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Local recurrence within the bladder and prostate was causing obstruction of his ureters with resulting abdominal and flank pain, difficulty urinating and hydronephrosis. Due to the size of the tumor, the obstruction could not be managed with ureteral stents, so he required bilateral nephrostomy tube placement to protect his kidney function. Managing the tubes in addition to the worsening pain he developed limited his day-to-day activity, and he was no longer able to attend elementary school.
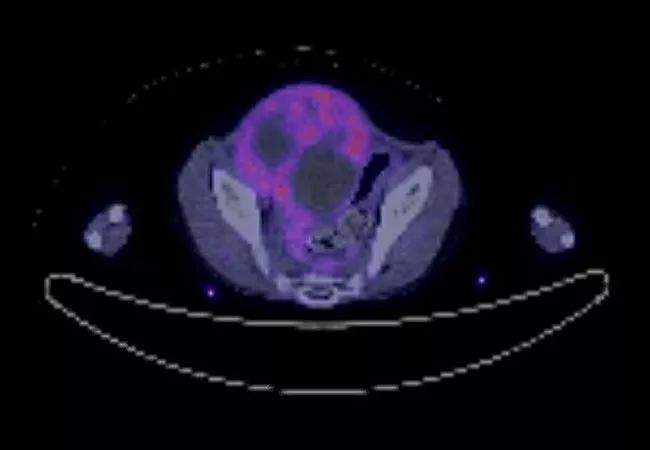
His local oncology team performed numerous scans, which showed that the mass was enlarging but had not metastasized. He was referred to Cleveland Clinic Children’s, and underwent evaluation with pediatric oncologist Peter Anderson, MD to review next line systemic therapy options. His tumor enlarged on multiple lines of systemic therapy, and in the absence of metastatic disease, he was referred for evaluation for surgical resection.
He underwent multidisciplinary surgical evaluation with urologic oncologist Nima Almassi, MD, pediatric urologist Audrey Rhee, MD and genitourinary reconstructive surgeon Hadley Wood, MD, of Glickman Urological & Kidney Institute. “One complicating factor was that the scans showed the mass was likely invading segments of small and large intestine and possibly the external iliac artery, so we sought the input of our pediatric and vascular surgeons,” says Dr. Almassi. “The mass was more than 15 centimeters and was protruding from his abdomen and perineum, making it painful to sit. Having progressed on systemic therapy and being ineligible for additional radiation, there weren’t other good options besides surgery.”
Advertisement
The care team and the patient’s parents determined that surgery would be the best chance of helping the young boy become cancer free, but it was understandably a challenge to gain buy-in from him, as facing a major surgery was frightening. The oncology and surgical teams worked to get to know the patient and his family and to develop a trusting relationship to help them navigate the challenges ahead. “Gaining the trust of a patient and their family was essential,” says Dr. Almassi. “Having a plan to not just evaluate treatment options, but to present the plan to a pediatric patient and his family and work through the natural anxieties and stress of undergoing a major surgery was critical to a successful outcome.”
The team realized the importance of developing a relationship with the patient, spending time with him and his family through virtual visits and on the phone prior to their trip to Cleveland, as well as in the hospital before the surgery and learning about his interests. They also engaged Child Life Services and the social work team at the Taussig Cancer Institute at Cleveland Clinic to distill information to a level that the patient could understand and accept. This helped in preparing him for surgery and getting him through the recovery.
“This is more than any child should ever have to bear, and he was amazing in terms of how he approached the surgery and recovery,” says Dr. Almassi. “He had phenomenal support from his parents, his siblings and his community back home, as well as support through our different teams in the clinic.
Advertisement
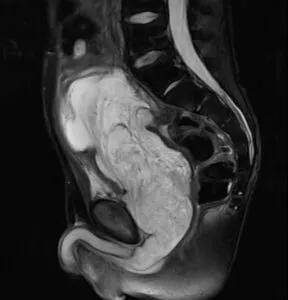
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/15d50c63-8ab5-475e-b5e6-66fe698a7d3e/22-CNR-3416210-Inset-800x833-bladder-cancer-2nd-image-288x300_jpg)
Preoperative MRI Pelvis – Sagittal view demonstrating 15cm mass involving the bladder, prostate, and bulbar urethra with invasion of the cecum. The mass demonstrated central necrosis.
The procedure required removal of the bladder, the prostate, a portion of the urethra, segments of intestine as well as a segment of the right external iliac artery. The surgery took approximately 14 hours, with Drs. Almassi and Wood performing a cystoprostatectomy, partial urethrectomy, and ileal conduit urinary diversion, Dr. Robertson performing a bowel resection of the involved intestinal segments and Dr. Khalifeh performing resection and reconstruction of the external iliac artery.
The 14- hour surgery was grueling, and came with risk of surgical complication. Fortunately, it was a success. The team was able to get negative surgical margins, and the patient did not have any major post-operative complications. Early in his recovery, the patient was ambulatory, and started walking around the hospital ward. By the time he went home, all the surgical drains and his nephrostomy tubes had been removed.
In the days following surgery, the medical team worked closely with the patient and his family, making sure they were comfortable with managing the stoma and ensuring he was progressing in terms of his activity and oral intake. Having an inconspicuous stoma appliance is much easier to manage than the two nephrostomy tubes the patient had lived with for the better part of a year.
While recovering from surgery, he received care from the surgical and medical teams, as well as physical therapy service and Child Life Services, who provided art and music therapy.
Advertisement
Two weeks after surgery, the patient and his parents were able to return home. Periodic scans and follow-ups are now coordinated through televisits between the teams in Pennsylvania and at Cleveland Clinic to monitor the patient’s kidney function and ensure there is no evidence of cancer.
Two months after surgery, the patient had experienced significant improvement in his functional capacity and quality of life. He has regained 13 pounds since the surgery. His cancer-associated pain had improved to the point that he was being weaned off of narcotics that he had long been reliant on, and he is able to be more active now that he is free of nephrostomy tubes. “His quality of life seems to have improved significantly, and he’s looking forward to going back to school in person,” says Dr. Almassi. “It’s incredible to see where he was when we first met him and where he is now. It’s been a blessing.”
“We knew it was going to be a very complex surgical treatment,” says Dr. Almassi. “Dr. Anderson and the whole oncology team managed the overarching care. Given how advanced the tumor was and knowing that we needed assistance with vascular reconstruction and bowel resection, having the expertise of different surgical teams allowed for a smooth course during the surgery as well as during the recovery. “
Dr. Almassi was quick to point out the family’s role in the recovery. “The way that his parents support and cared for their son while still taking care of their other children and managing their jobs and everything was incredible. An immense amount of credit has to go to the patient’s parents and to the patient himself.”
Advertisement
Advertisement

Oncologic and functional outcomes are promising, but selection is key

Findings confirm microbial variability, offer new potential treatment strategy

Research program sets the stage for clinical trials

Retrospective study finds acceptable cancer control among most histologic subtypes with intravesical therapy

What updated techniques, counseling and a changing workforce could mean

Approach offers a ‘middle ground’ between radical prostatectomy and active surveillance

AI histologic classifier reliably predicts clinical risk in men post-prostatectomy

Historic collaboration connects two Cleveland Clinic locations, enables real-time sharing of metrics and surgical progress