Retrospective study finds acceptable cancer control among most histologic subtypes with intravesical therapy
Cystectomy has been long regarded as the gold standard treatment for patients with nonmuscle invasive bladder cancer (NMIBC) with variant histology (VH). However, cancer control may be achieved with a less invasive, bladder-sparing treatment for many of the common VHs, according to a recent Cleveland Clinic study. These findings suggest that a new treatment paradigm could be at hand.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The authors reported their findings in Urologic Oncology: Seminars and Original Investigations.
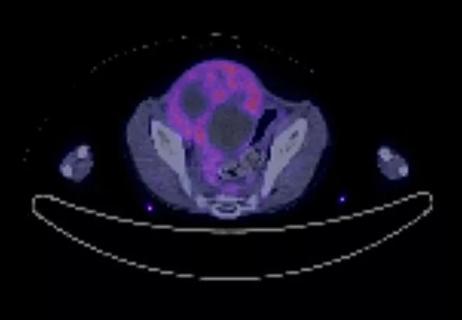
For the majority of new bladder cancer diagnoses—upward of about 70%—the disease is stage I, nonmuscle invasive and nonmetastatic. These patients are typically treated with transurethral resection bladder tumor (TURBT) surgery, an endoscopic resection, followed by intravesical therapy with Bacillus Calmette-Guérin (BCG) or chemotherapy.
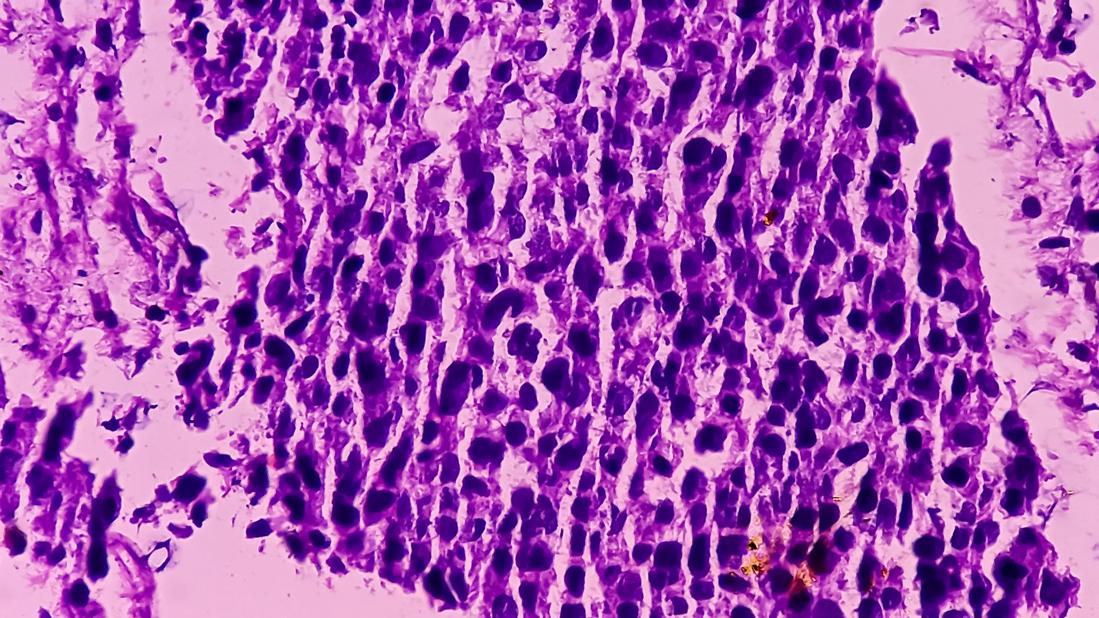
Those with VH, a subgroup defined by its divergent differentiation or histologic subtypes, have a rarer and higher-risk form of the disease. For these patients, Cleveland Clinic—and many other high-volume centers—recommend considering upfront radical cystectomy for treatment.
“Cystectomy is a highly effective treatment, but it’s also an invasive, life-changing surgery that can impact patients’ quality of life in a number of ways,” explains urologic oncologist Nima Almassi, MD, the study's lead author.
He adds, “While there are limited existing data on whether intravesical therapy is an effective means of cancel control for patients with variant histology, clinically, we have seen many of these patients do well,” an observation that set the stage for their investigation.
“The biggest concern is disease progression from stage I to II, III, or IV, as this increases the risk of cancer death,” notes Dr. Almassi.
The team performed a retrospective review of a Cleveland Clinic IRB-approved bladder cancer registry of patients treated at the institution from 2003 to 2020. Inclusion criteria included those with an NMIBC diagnosis, the presence of VH on a TURBT specimen, and at least one completed course of intravesical therapy with either intravesical BCG or chemotherapy.
Advertisement
The study examined those who were either ineligible for cystectomy or had declined the surgery. The VHs represented in their investigation included: micropapillary, nested, plasmacytoid, giant cell, lymphoepithelioma-like, sarcomatoid, glandular, and squamous differentiation.
Primary endpoints included evidence of cancer recurrence or progression, including muscle-invasive bladder cancer (MIBC), as well as cancer-specific and overall survival.
In total, the study included 90 patients with a median follow-up of 38 months. Most patients (72%) had T1 disease and received only intravesical BCG (83%) for treatment. Of the VHs in their analysis, glandular and squamous differentiation (26%) were the most common.
The study found acceptable cancer control with intravesical therapy among most variants.
Overall, recurrence within the bladder occurred in 48 of the patients (53%) with a median recurrence-free survival of 24 months. Five-year rates of progression to MIBC and distant metastasis were both 14%, respectively. Additionally, 26 patients (28%) eventually required cystectomy.
However, not all VHs responded uniformly to intravesical therapy. Significantly worse outcomes were noted in certain subtypes.
“Patients who harbored plasmacytoid or sarcomatoid variant, which we know is a very aggressive subtype of bladder cancer, did very poorly with intravesical therapy,” he says, reinforcing the need for aggressive treatment to improve cancer-specific survival. “Radical cystectomy should be prioritized for these patients.”
Advertisement
Patients with micropapillary differentiation had intermediate outcomes with intravascular therapy, consistent with what the authors expected. “These patients are at a higher risk of harboring nodal metastasis,” says Dr. Almassi, “which likely explains their higher risk of disease progression.” However, some patients with this VH remained disease-free, making it an intriguing area for further investigation and the focus of a clinical trial now underway at Cleveland Clinic.
Patients with other VHs such as glandular and squamous differentiation, responded favorably to intravesical therapy, according to the study. For these patients, a bladder-sparing approach should be a part of the conversation, the authors conclude.
While more data are needed to improve biomarkers and inform patient selection, the authors were encouraged overall by the oncological outcomes noted. Dr. Almassi notes it’s a critical step toward personalized bladder cancer care as experts continue to strike a balance between managing disease risk with functional outcomes and quality of life.
“This study offers data on the decision to deescalate treatment, but another consideration is how we are appropriately escalating treatment as well. As we fully transition to an era of personalized medicine, we need other predictive biomarkers to achieve optimal oncologic outcomes across all patients,” he says.
Advertisement
Advertisement

Oncologic and functional outcomes are promising, but selection is key

Findings confirm microbial variability, offer new potential treatment strategy

Research program sets the stage for clinical trials

What updated techniques, counseling and a changing workforce could mean
A recent case study illustrates surgical intervention for treating recurrent bladder cancer

Cleveland Clinic is first to use the device, known formerly as the UroMonitor

Retrospective study evaluates clinical upstaging during neoadjuvant treatment

Pediatric urologists lead quality improvement initiative, author systemwide guideline