Complex case in an elderly patient
A 75-year-old man traveled to Cleveland Clinic from New York in late 2019. He had been diagnosed with Crohn’s disease about two years earlier and was taking prednisone and mesalamine but not a biologic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
He was experiencing abdominal pain, distension, bloating, difficulty eating due to pain and weight loss. He vacillated between bouts of constipation and uncontrollable diarrhea with urgency and incontinence.
At his first visit, he met with Miguel Regueiro, MD, Chair of Cleveland Clinic’s Department of Gastroenterology, Hepatology and Nutrition. Although the patient had previously received a colonoscopy, Dr. Regueiro advised a second one because the prior gastroenterologist had encountered difficulty getting through a stricture in his sigmoid colon.
“That had implications, because in someone older with Crohn’s or inflammatory bowel disease, you always worry about cancer. We have ultra-thin scopes at Cleveland Clinic that are much different than we would use for a regular colonoscopy,” Dr. Regueiro explains.
In addition to his advanced age, the patient was also at higher medical risk because he had an implanted pacemaker for atrial fibrillation, and insulin-treated diabetes.
Dr. Regueiro performed the colonoscopy and was able to get the scope through the narrow part and through most of the colon, but not all the way up to the small intestine.
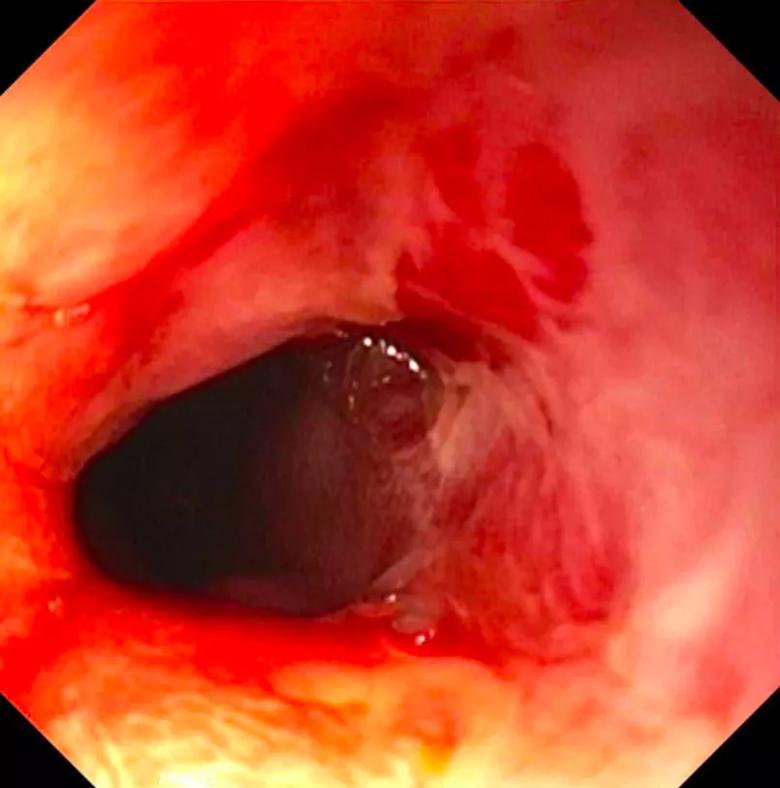
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c4cfcbbe-60ba-4241-9fa1-eb55be6ccca8/20-DDI-1890388-Crohns-Stricture-Colon_jpg)
Nonetheless, “it didn’t look like a cancer to me, and I didn’t see a lot of Crohn’s disease higher up in his colon. He did have a severe stricture in his sigmoid colon, with a lot of narrowing scar tissue that had built up. In Crohn’s, the medications are good at reversing inflammation but when the body forms a stricture, we don’t yet have a medication for that,” says Dr. Regueiro.
Advertisement
Thus, the patient was at risk for a full bowel blockage and perforation. “This is a challenging problem in anyone, let alone a man in his mid-70s with other comorbidities,” he says.
So, at that same visit, the patient and his wife met with Dr. Regueiro, Scott R. Steele, MD, Chair of Colorectal Surgery, a nutritionist, a nurse practitioner and an ostomy nurse in case an ostomy would be needed. Because of his pacemaker and diabetes, cardiology and endocrinology were consulted as well.
Dr. Steele notes, “Dr. Regueiro and I have clinic on the same day so the patients can see both of us, then we meet and discuss the way forward.”
Dr. Steele performed an open ileocolic resection with ileocolic anastomosis as well as transverse colon stricture anastomosis with hand-sewn end-to-end anastomosis. The procedure also involved removing the narrowing in the sigmoid colon and accompanying fistula. In addition, Dr. Steele performed splenic flexure mobilization and diverting loop ileostomy.
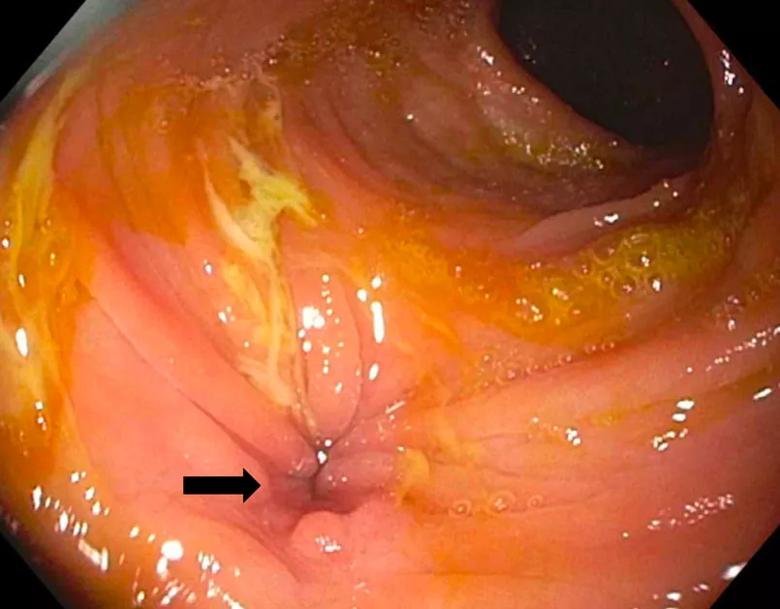
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f57a38e6-de34-40de-9e97-a18c6349b625/20-DDI-1890388-Colon-Fistula_jpg)
“He ended up having several strictures and fistulas that were more extensive than what the initial imaging had shown. He also had a chronic perforation of his descending colon that his body had walled off. Nonetheless, we were able to take care of it all. Thankfully, he had no surgical or post-op complications,” Dr. Steele says.
During his subsequent week-long hospital stay, a nutritionist taught the patient and his wife about the low-FODMAP diet, which minimizes fermentable oligosaccharides, disaccharides, monosaccharides and polyols, all of which exacerbate bowel symptoms.
Advertisement
After discharge, the patient met several times with team members via telehealth visits. Cleveland Clinic nurses also called the patient frequently to check on him.
The patient returned three months later for ileostomy closure, which went smoothly and involved a shorter stay.
The patient had been scheduled to return during the first half of April, but that visit was converted to virtual due to the pandemic. Luckily, “Cleveland Clinic had embraced the telemedicine platform for a while. The team members have been able to reach out to him without difficulty since the pandemic hit,” Dr. Steele says.
Regueiro says that since the surgery, the patient has no more pain, is able to eat normally, and has normal bowel movements. At this time, he’s not taking any Crohn’s medications. “Time will tell if he will need future Crohn’s medications, and that will depend on his colonoscopy in six months.”
This case illustrates “the importance of having experienced providers who work very well together taking care of complex disease processes in a multidisciplinary pathway to not only address the here and now but also look toward the future to have an individualized treatment program for each patient,” says Dr. Steele.
He anticipates that will remain true even during the COVID-19 pandemic. “When the world changed, we had the platforms in place to easily incorporate and adapt to take care of our patients even when they can’t come in and see us.”
Advertisement
Advertisement
Benefits of neoadjuvant immunotherapy reflect emerging standard of care
Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence
Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors
Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling
Potentially cost-effective addition to standard GERD management in post-transplant patients
Findings could help clinicians make more informed decisions about medication recommendations
Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care
Retrospective analysis looks at data from more than 5000 patients across 40 years