Treatment involved checkpoint inhibitor, surgery and intravesical therapy
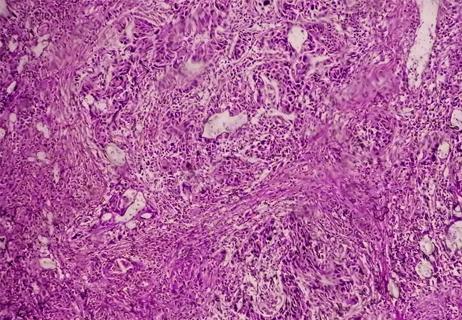
Historically, metastatic upper track urothelial cancer had a poor prognosis, with survival often less than a month. After undergoing standard chemotherapy for the disease with only a marginal response, a man in his 60s came to Cleveland Clinic Cancer Center for treatment. The disease had already spread to his lymph nodes, liver and lungs.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A team of clinicians met to discuss the patient. Medical oncologist Timothy Gilligan, MD, started the patient on the antibody drug conjugate enfortumab vedotin. The patient became an early participant in a trial of the medication, which is now FDA approved for treating advanced urothelial cancer.
The treatment has a different mechanism than standard chemotherapy. With this treatment, a monoclonal antibody to nectin protein, which is prevalent in urothelial cancer, and then releases the chemotherapy to kill those cells. In this way, the drug is delivered closer to the source of cancer cells, providing somewhat less toxicity than standard chemotherapy. The patient had a considerable response to this treatment.
"Clinical trials were just starting at the time the patient began treatment with enfortumab vedotin," says Cleveland Clinic Director of Urologic Oncology Christopher Weight, MD.
"Now that the trials have matured, they've shown that on average, patients have longer survival. It seems there is a subset of patients with a combination of immunotherapy and chemotherapy that have longer term survival and response rates."
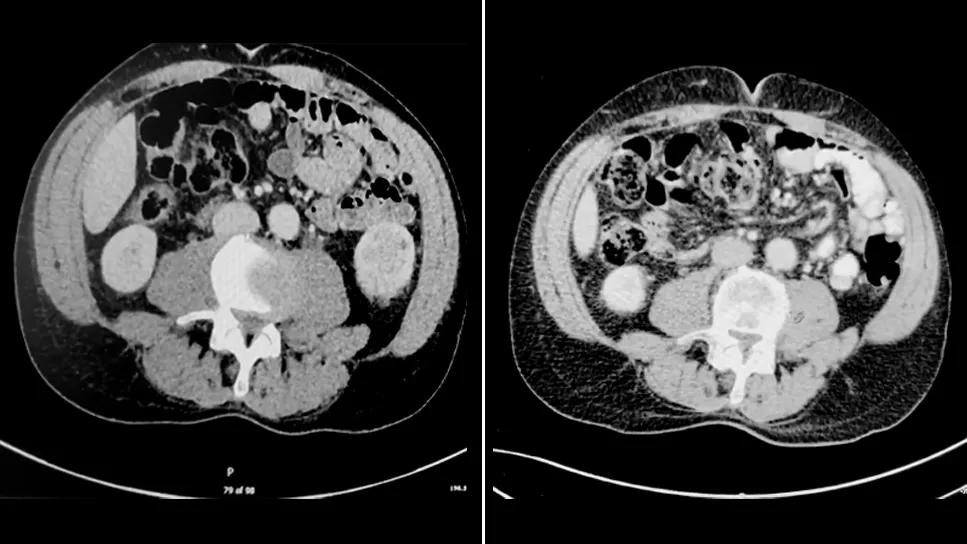
Although this patient had a robust response to the treatment, the tumor in his left kidney remained. The team then consulted together, met with the patient and decided on consolidation surgery. Dr. Weight performed the nephroureterectomy laparoscopically.
This robot-assisted procedure involved removal of the kidney, most of the ureter as well as lymph nodes. Due to the antibody drug conjugate treatment the patient had, the lymph nodes that were removed no longer showed signs of cancer.
Advertisement
Roughly five years later, the patient had a recurrence, with several tumors in his bladder.
"This type of cancer is notorious for growing where it lands," explains Dr. Weight. "It started in his kidneys but over time, microscopic cells were washing down into the bladder."
Drs. Gilligan and Weight consulted with a wider team in their Tumor Board about the appropriate approach and the patient's needs. "We've discussed his case several times because he kept breaking traditional paradigms," says Dr. Weight. "We found it crucial to have clear communication boundaries, multi-departmental understanding of the tools needed at each point in the disease state as well as a determination of which clinician had the right tools to best serve the patient.”
The team felt that bladder management would be the next appropriate step, and the patient underwent surgery to ablate the cancer cells. Several weeks after the procedure, the team administered intravesical therapy for the subsequent six weeks. This therapy stimulates the immune system as a preventative measure to stave off additional tumor cells.
The patient fared well. However, several months later, he experienced a recurrence in the bladder, and received additional surgery and intravesical therapy. In the latest CT scan and cystoscopy performed afterwards, there was no evidence of disease. "It was a joyous and a solemn moment when I met with him and his wife," says Dr. Weight. "This is the first time in a long time that he's not having any sort of cancer treatment."
Advertisement
The patient will continue to receive maintenance intravesical therapy every six months as a protective measure, with regular scans and cystoscopies performed every three months. "It's incredible that this man who was given months to live is actually disease free," says Dr. Weight.
Advertisement
Advertisement

Enfortumab vedotin plus pembrolizumab benefited patients, regardless of biomarker expression

Platinum-eligible phase 3 trial of enfortumab vedotin and pembrolizumab yields ‘unprecedented data’

Enfortumab plus pembrolizumab reduced risk of death by 53% compared with platinum-based chemotherapy
Potential treatment option for patients who are ineligible for cisplatin

Findings could help with management of a common, dose-limiting side effect

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting