Prompt, multidisciplinary care helps navigate the complexities of a rare condition
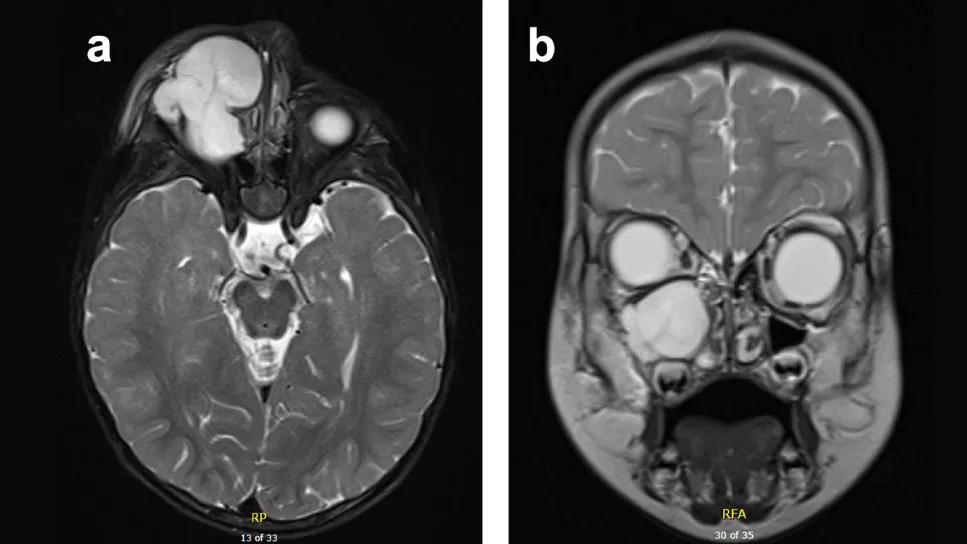
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c5f9bf1d-4557-4d2a-8314-ef48e1a188d9/Ped-Sinonasal-Myxoma-Extraconal-Intraorbital-Ext-hero)
T2 Magnetic Resonance Imaging (MRI) of maxillary sinus mass with extraconal intraorbital extension
Sinonasal myxoma — an exceedingly rare, benign tumor that occurs in the nasal and sinus cavities — can be particularly challenging to diagnose due to its subtle and nonspecific symptoms. These include nasal obstruction, facial pain, epistaxis and headaches. In some cases, the tumor can extend beyond the sinuses, affecting surrounding structures, such as the eye sockets, which leads to more noticeable facial changes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Due to the rarity of this condition, sinonasal myxoma requires a high clinical index of suspicion. While benign, its potential to grow and invade nearby areas highlights the importance of early detection and precise treatment.
Rachel Georgopoulos, MD, a pediatric otolaryngologist at Cleveland Clinic, recently cared for a young patient with infraorbital extension of sinonasal myxoma. During the American Academy of Otolaryngology-Head and Neck Surgery Annual Meeting, she shared her experience with this patient, detailing diagnosis, treatment and lessons learned.
An 18-month male presented to Cleveland Clinic with a three-month history of progressively worsening right facial swelling on the infraorbital/right cheek.
During the physical examination, Dr. Georgopoulos observed facial swelling in the right infraorbital region with no overlying erythema or induration. A mass in the maxillary sinus with extraconal intraorbital extension was found via magnetic resonance imaging (MRI). Positron emission tomography (PET) scan showed a non-FGD avid expansile large soft tissue mass in the right maxillary sinus.
Following imaging, an incisional sublabial biopsy confirmed the low-grade myxoid spindle cell neoplasm, a finding consistent with sinonasal myxoma. “The tumor was growing rapidly and had broken through the inferior orbital floor,” Dr. Georgopoulos notes. “We were concerned about a potential compression of the eye and poor vision. Luckily, he showed no signs of loss of vision at the time, but treatment was initiated quickly.”
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/027227af-0ecb-47a7-9a5d-5ee2c60c3f9c/Ped-Sinonasal-Myxoma-Extraconal-Intraorbital-Ext-inset)
Above: Computed Tomography (CT) scan of facial bone demonstrating mass involvement of right orbital rim. At top of page: T2 Magnetic Resonance Imaging (MRI) of maxillary sinus mass with extraconal intraorbital extension
Dr. Georgopoulos collaborated with her colleague Brandon Prendes, MD, a reconstructive head and neck surgeon at Cleveland Clinic’s Department of Otolaryngology-Head and Neck Surgery, to treat this patient. She performed a complete excision of the facial mass via a Weber Fergusson incision and maxillectomy with resection of the orbital floor and rim. “A Weber Fergusson incision,” Dr. Georgopoulos explains, “runs along the side of the nose and offers favorable cosmetic healing.”
The tumor had destroyed the entire inferior orbital floor, so reconstruction was crucial to prevent the eye from sagging, according to Dr. Georgopoulos. “Dr. Prendes used a graft I harvested from a right rib to create a new orbital floor to support the eye, along with a small implant to support the orbit. Additionally, an anterolateral thigh (ALT) flap, a portion of muscle from the leg, was used to fill the large space left by the tumor.”
At 8-months follow-up, no functional deficits, including no issues with dentition or vision, were observed. An MRI showed no evidence of a recurrent tumor. Dr. Georgopoulos says, “The patient had an excellent cosmetic outcome and continues to do well with no complaints or concerns.”
Successful treatment in this case required a multi-disciplinary approach, resulting in excellent tumor control and functional/cosmetic outcome, according to Dr. Georgopoulos and colleagues, who also note that sinonasal myxoma should remain on the differential for a child presenting with a sinonasal-based facial mass.
Advertisement
This case is unique, not only due to the rare nature of sinonasal myxoma, but also because of the reconstruction approach taken by the team at Cleveland Clinic. “The intricacy of a reconstruction like this stands out, particularly in children, where growth is a major factor,” notes Dr. Georgopoulos.
“Unlike adults, where simpler approaches, such as plates, may suffice, pediatric cases require more nuanced techniques,” she explains. “In this case, we used a rib graft, which has the potential to grow with the child. This adds a layer of complexity to the reconstruction, making it more challenging compared to adult cases where growth is not a concern.”
This case study underscores several valuable takeaways, including the importance of expeditious care. Even benign tumors can be locally aggressive and create significant morbidity, Dr. Georgopoulos notes. In this case, for instance, the patient faced the complete loss of his orbital floor, highlighting the need for swift and careful management.
“Additionally, the case emphasizes the importance of a cohesive surgical team, where both tumor resection and reconstruction are equally critical,” concludes Dr. Georgopoulos. “Using a rib graft to reconstruct the orbital floor in pediatric patients is less common but proved successful in this case, offering new insights for future pediatric reconstructions.”
Advertisement
Advertisement
An expert’s take on evolving challenges, treatments and responsibilities through early adulthood
Comorbidities and medical complexity underlie far more deaths than SUDEP does
Case-control study yields evidence of epigenetic aging in pediatric-onset MS
Leaders of the Pediatric Cancer Committee discuss new accreditation
Despite advancements in the specialty, patient-centered care needs to remain a priority
How innovations and advancements in skull base surgery are improving outcomes
A commitment to sharing expertise has fostered a global exchange of ideas
Surprising X-ray results explain a snoring sound heard during breathing